lane Dermatology
WE ARE HERE FOR YOU
Nothing is more important than your health.
If it's time for your annual check-up or you need medical attention, give us a call.
To request an appointment, call 225-658-4065.
For Emergencies, please call 911.
-----------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------
Baton Rouge Area Dermatology
At Lane Dermatology, we care about your skin as much as you do.
Dr. Ashley Record and Dr. Jessica LeBlanc are committed to long-term skin care health for people of all ages including children and teens.
Whether you need an annual screening or immediate attention for an ailment, as experienced, board-certified dermatologists, we treat most skin, scalp, and nail conditions.
Ask us about Botox services and other skin care options!
Common Conditions & Diseases We Treat
Acne
Acne is a very common skin problem that shows up as outbreaks of bumps often referred to as pimples or zits. This usually appears on the face, neck, back, chest, and shoulders. Acne can be a source of emotional distress, and severe cases can lead to permanent acne scars. Anyone can have acne, but teenagers are most prone because of the surging adolescent hormone levels. Women may get acne when their hormone levels change during pregnancy, just before a menstrual cycle, or when starting birth control pills.
Acne begins when the pores in the skin become clogged and can no longer drain sebum (an oil made by the sebaceous glands that protects and moisturizes the skin.) The sebum build-up causes the surrounding hair follicle to swell. The plugged pores form blackheads and whiteheads, pimples and deeper lumps (cysts or nodules).
Control of acne is an ongoing process. Keep skin clean, wash your face with a mild cleanser twice a day. Avoid harsh astringents and hard scrubbing of the skin. Don't squeeze or pick at blemishes. Limit sun exposure and use an oil-free sunscreen, such as a gel or light lotion. Choose skin care products and cosmetics labeled "non-comedogenic" (does not promote acne).
Almost all cases of acne can be effectively treated. The goal of acne treatment is to heal existing lesions, stop new lesions from forming, and prevent acne scars. Medications vary, depending on the type of acne you have. Mild acne may respond well to a topical retinoid alone. Moderate acne may respond better to a combination of a topical retinoid with an antibiotic or other medication. Severe acne with scarring may need treatment with isotretinoin, the active ingredient of Accutane. Chemical peels, slushes, and laser treatments can also help clear up acne.
Allergy Testing (Patch Testing for Contact Dermatitis)
Skin Patch Testing
Lane Dermatology is offering patch testing to identify substances that may be causing a skin rash, or contact dermatitis.
The patch testing procedure is simple and painless. The test involves applying patches of various diluted allergens onto the skin, usually on the back. Patches are worn for approximately 2 days and then removed. The area of skin that was tested will be evaluated by the dermatologist 4 days after the patches are removed to see if any skin rashes are present, which confirm an allergy/allergies.
The skin patch test differs from a skin prick test in that if focuses on contact skin allergens as opposed to reactions from food consumption or airborne allergens. It is a safe, effective way to diagnose contact allergies to learn which everyday ingredients, chemicals, soaps, fabrics, metals, or other materials to avoid.
Click any of the topics below to learn more:
- Contact Dermatitis Overview
- Itchy Rash: Could it be Contact Dermatitis?
- Signs & Symptoms
- Diagnosis & Treatment
- Causes
- Tips for Managing
CONTACT DERMATITIS OVERVIEW
If your skin reacts to something and your dermatologist suspects you’re having an allergic reaction, your dermatologist will try to find what’s causing the reaction. To a dermatologist’s trained eye, this may be obvious. A rash from poison ivy or an e-cigarette can be easy to spot.
Other causes can take time to find. More than 15,000 substances can cause an allergic skin reaction. It’s also possible that you have developed an allergic reaction to more than one substance.
If your skin continues to itch and develop rashes, your dermatologist may recommend a medical test called patch testing. Some dermatologists offer patch testing in their office. If your dermatologist does not offer patch testing, you will be referred to another doctor or medical office.
Patch testing differs from a skin prick test. When you get a skin prick test (or scratch test), your doctor checks for an immediate reaction. Skin allergies tend to develop in hours or days, so a patch test checks for this type of skin reaction.
Patch testing can find what’s causing an allergic reaction on your skin
The patches are normally applied to your back and must be left in place for a period of time.

What’s involved in patch testing?
If you have patch testing, here’s what to expect:
- Your dermatologist will place small amounts of allergens (what can cause an allergic reaction) on your skin and cover each allergen with a patch. The purpose is to see if any allergens cause your skin to react.
- You will leave the patches on your skin for 48 hours. If your skin reacts during this time, it may feel itchy or sore. Despite this, it’s essential to keep the patches on your skin so that you can get accurate results. If you remove the patches, loosen them, or get them wet, you’re likely to get inaccurate results.
- After 48 hours, you will return to your dermatologist’s office. Your dermatologist will remove the patches. If your skin reacted to any of the allergens, your dermatologist can tell you what caused the reaction.
- After 4 to 7 days, you will see your dermatologist again. It’s essential to keep this appointment because it can take time for your skin to develop an allergic reaction.
If patch testing reveals that you have one or more allergies, your dermatologist will create a treatment plan. You may need to apply medication to help the rash heal. All treatment plans include instructions to help you avoid what’s causing your skin to react.
Because so many things that touch our skin can cause contact dermatitis, it’s possible that the first round of patch testing fails to find what’s causing your skin to react. If this happens, your dermatologist may recommend testing other substances.
Many people develop an allergy to a substance that they work with often. Job-specific allergies are so common that patch testing is available for certain industries. For example, certain patches can be applied to people who work as a florist or dental technician. This is called expanded patch testing. It finds about 80% of allergens.
Possible side effects from patch testing
The patches irritate some people’s skin. If you have irritated skin, it usually clears on its own in a few days. People who have darker skin tones may see lighter or darker skin where the patches were applied to their skin. This discoloration will also clear on its own.
If you have psoriasis, the patches can trigger a psoriasis flare-up.
It’s rare to have a serious side effect from patch testing. A few people have developed an infection or life-threatening allergic reaction. When someone develops a life-threatening allergic reaction, this occurs within 30 minutes of applying the patches.
Signs of a life-threatening allergic reaction
Signs of a life-threatening allergic reaction are swelling, nausea, vomiting, and difficulty breathing. If you notice these signs, get immediate medical care.
What you do while wearing the patches affects your results
To get accurate results, you must follow the instructions given to you. If you scratch the patches or take a shower, the test will likely miss something that’s causing your skin to react.
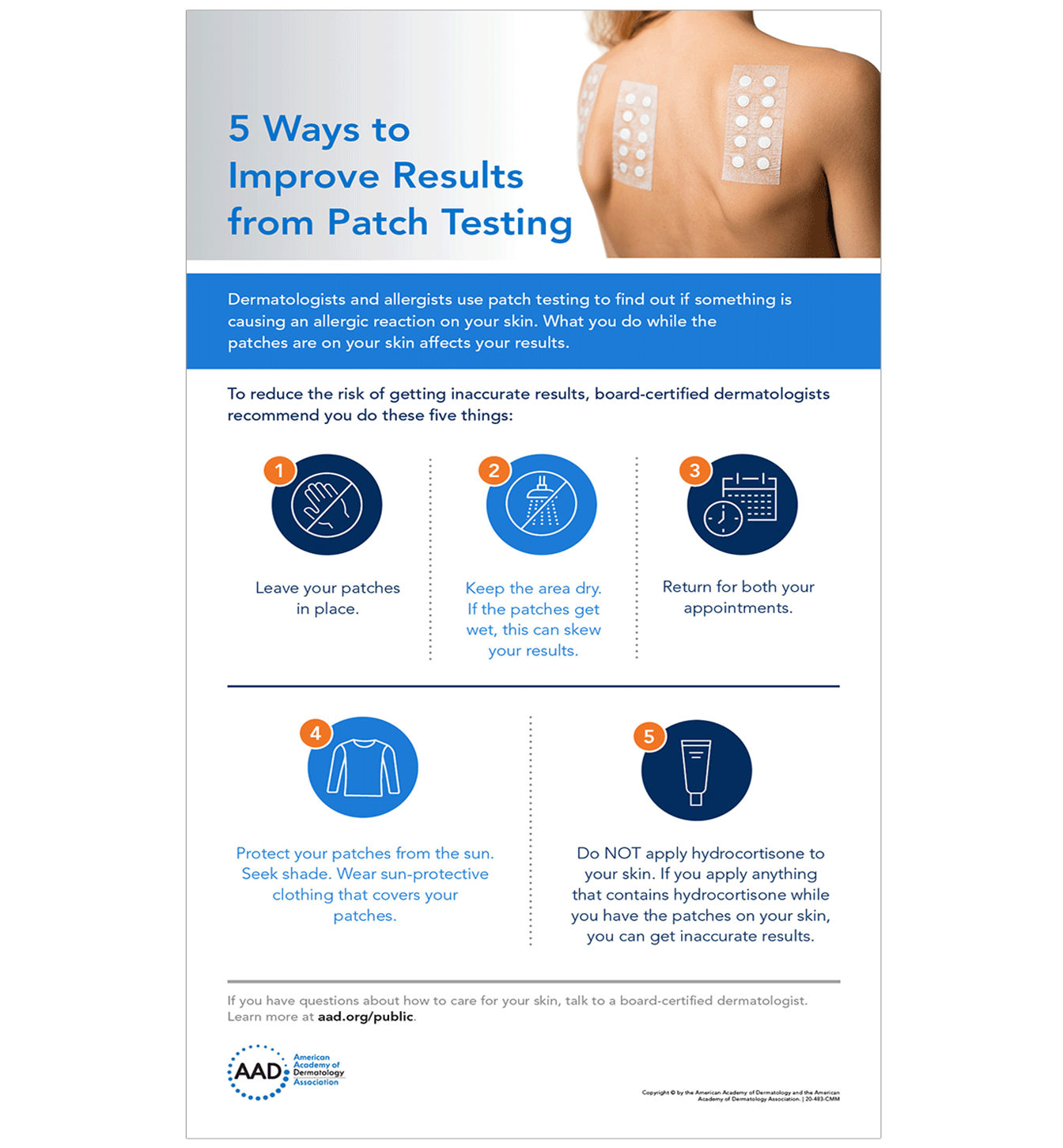
Infographic: 5 ways to improve results from patch testing
To reduce your risk of getting inaccurate results, follow these five tips that dermatologists give their patients.
Patch testing can find what’s causing your rash
The results from your patch test can help uncover what’s causing your skin to react.
Once your dermatologist knows the cause (or causes) of your contact dermatitis, your dermatologist will create a plan to help you avoid what’s causing your rash.
For many patients, the results from patch testing significantly improve their lives. Once you know what’s causing your itchy rash, you can avoid it. This often leads to clearing.
SIGNS AND SYMPTOMS OF CONTACT DERMATITIS
You can develop contact dermatitis on any part of your skin that touches something which either irritates your skin or causes an allergic reaction. Because we touch most things with our hands, contact dermatitis often develops here.
If you have an allergy to fragrance, which is common, you may develop contact dermatitis where you apply a personal care product. The face, neck, underarms, scalp, and tops of feet are also common places to develop contact dermatitis. However, contact dermatitis can appear anywhere on your skin.
When signs and symptoms appear, you may have:
- Itchy skin (often intense)
- Rash (skin discolored, swollen, and hot)
- Excessively dry skin that may crack
- Tender skin
- Burning or stinging
- Hives (round welts on the skin that itch intensely)
- Fluid-filled blisters
- Oozing blisters that leave crusts and scales
Itch, burning sensation, or pain
Before the rash appears, you may feel an intense itch, burning sensation, or pain. These symptoms often continue after the rash appears.

Itchy rash
This man developed contact dermatitis after using a spice-scented deodorant. The itchy rash cleared soon after he stopped applying the deodorant.

Swelling and a rash
The product that causes contact dermatitis doesn’t have to touch your skin for long. This woman had an allergic reaction to shampoo, which only touched her eyelid when she rinsed it off in the shower. Because the skin on the eyelid is thinner than elsewhere, this is a common place for contact dermatitis to develop.

Intensely itchy rash of bumps and fluid-filled blisters
Poison ivy caused the rash of itchy bumps and fluid-filled blisters shown here. Many people develop an allergic reaction on their skin when it touches poison ivy, poison oak, or poison sumac.

When bumps and blisters appear, your skin may feel swollen and blistered or dry and bumpy.
Painful sores
This woman was working with fiberglass, which irritated her skin and caused the painful sores.

Sores leak fluid
If the sores break open, they can leak fluid. The sores shown here are due to severely irritated skin caused by handling fish.

Rash appears after sunlight hits the skin
By seeing a dermatologist, this woman discovered her constantly itchy rash and swollen skin were caused by a product that contained oil of bergamot. When the oil on her skin reacted with sunlight, this rash appeared.

Rash comes and goes
If you only occasionally touch what’s causing contact dermatitis, the rash can come and go. Because an allergic reaction can take time to appear, it can take a bit of detective work to figure out what’s causing the rash. By seeing a dermatologist, this woman discovered that she has a nickel allergy. The necklace shown in this picture contains nickel, which is causing her rash.
Jewelry often contains nickel. This metal is also found in cell phones, laptops, and other tech devices.

Thickened, dry, cracked, and flaky skin
If you continue to touch what’s causing the contact dermatitis, your skin often thickens, becomes scaly, and develops deep cracks. This usually happens when someone needs to work with chemicals, such as hair dyes, cement, or solvents. The long-standing contact dermatitis shown here appears on the hand of a massage therapist who uses essential oils to treat clients.

Contact dermatitis can develop anywhere on your skin
While contact dermatitis often develops on the hands, it can appear anywhere on your skin, including feet, lips, or groin area. Sometimes, the cause never directly touches your skin. For example, shoes can cause an allergic reaction on feet covered by socks.
Other times, the skin next to something that causes an allergic reaction may not rash. You may develop the rash elsewhere. For example, some people develop an allergic reaction to chemicals used in nail polish or artificial nails. Instead of developing a rash on their hands or feet, some people get a rash on their eyelids.
The skin around the eye is thin. If you’re allergic to something on your fingers, such as an ingredient in a nail polish, briefly touching the skin around the eye could cause a rash.
Contact dermatitis caused by shoes
This man developed a serious allergic reaction to a resin in his shoes.

The rash around this woman’s eye was caused by an allergic reaction to her artificial nails.

While rare, the rash on a person’s skin can also be caused by something inside their body. For example, some people develop an allergic reaction to a metal in an artificial hip or knee. A few patients have developed an allergic reaction to their pacemaker.
DIAGNOSIS AND TREATMENT OF CONTACT DERMATITIS
By gathering the right information and studying it, dermatologists have found causes of contact dermatitis that often surprise their patients. Examples include:
- Cleaning supplies used to clean the toilet seats at a patient’s workplace
- Incense that a patient’s roommate burns
- Wedding ring that a patient has worn for more than a decade
How do dermatologists diagnose contact dermatitis?
When a dermatologist suspects that contact dermatitis is causing your rash, a dermatologist will:
- Examine your rash(es) carefully
- Ask you questions about your health, job, hobbies, and everyday activities, when necessary
- Test your skin to see if you are allergic to anything that may cause a rash, when necessary
The questions that your dermatologist asks can play a key role in finding out if you have contact dermatitis. For this reason, it’s important to think carefully about your answers.
When talking with your dermatologist be sure to mention:
- All the skin, hair, and nail care products you use
- Whether you apply skin, hair, or nail care products to someone you care for, such as a child or an elderly parent
- When the rash appears
Your dermatologist may ask for details about your work. Many people develop contact dermatitis at their workplace. This is a common problem for hairstylists, health care workers, florists, chefs and other food service workers, people who work in manufacturing or agriculture, and mechanics.
After examining your skin and listening to your answers, your dermatologist may be able to figure out what is likely causing your rash. For example, your dermatologist can often quickly tell if poison ivy or an e-cigarette is the cause. To the trained eye, both leave telltale signs.
If an ingredient in your skin care products is causing your rash, it can be difficult to know which ingredient is responsible. Your dermatologist may have you stop using certain products for a while to see if the rash clears.
Sometimes, your dermatologist will recommend patch testing.
Finding the cause of contact dermatitis often requires a detective-like approach
So many things that touch your skin can lead to contact dermatitis.

How do dermatologists treat contact dermatitis?
The best way to treat contact dermatitis is to avoid what’s causing it. If you can avoid the cause, the rash and symptoms will go away.
Once you know what’s causing your contact dermatitis, learning what to avoid can be straightforward. For example, if poison ivy caused your rash, avoiding plants that contain urushiol (what causes the allergic reaction) can prevent another rash. When you cannot avoid these plants, your dermatologist can teach you how to protect your skin.
Other times, avoiding what causes your contact dermatitis can be more difficult. For example, if you’re allergic to nickel, hundreds of things that touch your skin could cause a rash. Everyday objects that may contain nickel include cell phones, buttons and zippers on clothing, and jewelry.
Your dermatologist can help you develop a realistic plan for avoiding what causes your rash. Learning what to do may take time. Taking the time to learn what can cause your rash will help you feel more comfortable and develop fewer rashes.
Because so many things can irritate the skin or cause an allergic reaction, it’s not always possible to find the cause. To complicate matters, some people develop allergies to many different things. When this happens, treatment can help.
Medication and other treatments for contact dermatitis
To relieve your discomfort and help clear the rash, your dermatologist may include one or more of the following in your treatment plan.
Rash: Medication prescribed by your dermatologist that you apply to the rash.
Rash that covers much of your skin: Medication that works throughout your body, such as prednisone. This medication can reduce the swelling and clear the rash. Most people get relief within 12 to 24 hours.
Itch relief: Cool compresses. Your dermatologist will explain how to use these.
Open sores that leak: Calamine lotion or colloidal oatmeal baths
Follow the directions that come with your medication
Some people are tempted to quit a medication when they see the rash clear. This can cause a serious problem. If you’re taking prednisone, suddenly stopping the medication can cause the rash to reappear. This is called a rebound rash, and it can be more serious than the rash that cleared.
When a patient continues to have rashes
While medication can help clear the rash, a few people continue to develop new rashes. Having rashes most of the time can interfere with life. To help their patients feel more comfortable and lead fulfilling lives, dermatologists can prescribe long-term medication.
These medications help to calm your overactive immune system. Your dermatologist may prescribe methotrexate or another medication.
Another option may be a treatment called phototherapy. To get this treatment, you will need to go to your dermatologist’s office or a hospital a few times a week for several weeks. During this treatment, your dermatologist uses light to help clear your skin and calm down your immune system.
Some patients get relief by applying medication to their skin when they get a rash.
Your dermatologist will consider your individual needs and prescribe an appropriate treatment.
If you continue to have rashes after trying a treatment, tell your dermatologist. When one treatment fails, another may work.
WHAT CAUSES CONTACT DERMATITIS?
There are two main types of contact dermatitis. The rash and other symptoms of contact dermatitis develop when something either:
- Irritates your skin, causing irritant contact dermatitis
- Triggers an allergic reaction, causing allergic contact dermatitis
Irritant contact dermatitis: When something injures and then irritates your skin, it causes this type of contact dermatitis. Common irritants that can injure your skin, causing irritant contact dermatitis, include:
- Detergents and bleach
- Plants
- Fruit juice
- Hand sanitizers
- Soaps
- Gasoline and diesel oil
- Disinfectants
- Fertilizers and pesticides
- Chemicals used to remove grease, oils, and cutting fluids
The above list gives you an idea of what can irritate your skin. It’s important to know that these are just a few of the many things that can irritate your skin. Under the right circumstances, even water can cause irritant contact dermatitis.
For example, if you dip your hands in water throughout the day and do this nearly every day, the water can strip away your skin’s protective barrier. Without a protective barrier, you have injured skin. If you continue to injure your skin by dipping your hands in water frequently, you develop irritant contact dermatitis.
Frequent handwashing can also cause irritant contact dermatitis. To reduce your risk, use mild soaps and cleansers. Applying a fragrance-free hand cream after each hand washing also helps.
Skin care products are a common cause of contact dermatitis
Even “natural” or “clean” skin care products can cause a skin reaction.

Allergic contact dermatitis: If what touches your skin causes an allergic reaction, you develop this type of contact dermatitis.
It can be difficult to figure out what’s causing allergic contact dermatitis because it takes time for the rash to appear. When your skin touches an allergen (what you’re allergic to), this triggers your immune system. A series of events occur inside your body before your skin reacts. For this reason, it can take hours or days before you develop a rash and symptoms.
While there are more than 15,000 allergens, some are more common. The most common causes of allergic contact dermatitis are:
|
Allergen |
Where it's found |
|
Nickel |
Jewelry (including wedding rings and body piercings), cell phones, foods, and e-cigarettes |
|
Fragrance |
Perfume, skin care products, shampoos, and many other personal care products |
|
Balsam of Peru |
A fragrance used in cosmetics and personal care products, used in “unscented” products to cover up a fragrance, found in many foods (spices, ketchup, beer, wine, colas, chocolates, and more) |
|
Latex |
Medical supplies, including gloves (If you have a latex allergy, some foods like avocados, bananas, and kiwis can cause a flare-up.) |
|
Urushiol |
Found in the sap of poison ivy, poison oak, and poison sumac |
Some people only develop contact dermatitis after certain chemicals touch their skin and then ultraviolet (UV) light, such as sunlight, hits their skin. The rash only appears where the UV light hits their skin. Dermatologists refer to this type of allergic contact dermatitis as photocontact dermatitis.
Some people have a higher risk of developing contact dermatitis
While it’s possible for anyone to develop contact dermatitis, some people have a greater risk.
If you have a skin condition that lessens your skin’s ability to protect you from germs and other invaders, you have a greater risk. Conditions that cause this include atopic dermatitis (AD), stasis dermatitis, and leg ulcers. When your skin is less able to protect you, it’s easier for something to irritate your skin or trigger an allergic reaction.
People who work in certain jobs also have a higher risk. Anyone who dips their hands in water throughout the day or works with harsh chemicals has a higher risk.
As for specific jobs, studies show that people who work in one the following industries or jobs have a higher risk of developing contact dermatitis:
- Health care workers
- Food service workers, chefs, and bartenders
- Construction workers
- Cosmetologists (including hairstylists, nail technicians, makeup artists)
- Florists
- Machinists
- Mechanics
- Agricultural workers
- Natural resources and mining
- Manufacturing
In the United States, contact dermatitis is one of the most common diseases caused by the workplace.
What can get rid of contact dermatitis?
If you can figure out what’s irritating your skin or causing an allergic reaction, you can get rid of the contact dermatitis. To heal your skin, you need to avoid what’s causing your skin to react.
For example, if you smoke e-cigarettes and have a rash on your lips and the hand that you hold the e-cigarette with, the cause is probably e-cigarettes. If you stop using e-cigarettes and the rash clears on its own, you’ve likely found the cause.
Finding the cause isn’t always easy. If you continue to have a rash, see a board-certified dermatologist. This doctor can tell you whether you have contact dermatitis, an infection, or another skin condition.
A dermatologist can also help when you cannot avoid what’s causing your contact dermatitis. For example, if you work with harsh chemicals or need to wash your hands frequently throughout your workday, a dermatologist may recommend a glove that can protect your skin or a skin care product that helps.
TIPS FOR MANAGING CONTACT DERMATITIS
If you have contact dermatitis, the right skin care and prevention strategies can help heal your skin and prevent another itchy, painful rash. Here are the tips that dermatologists give their patients who have contact dermatitis.
- Avoid what’s causing your rash. To heal your skin and prevent another rash, you need to: 1) Know what’s causing your rash and 2) Avoid touching what causes it.
For example, if you have an allergy to nickel, you need to know what often contains nickel and how to avoid it. You’ll find five tips that can help you avoid nickel at, Nickel allergy: How to avoid exposure and reduce symptoms.
If you’re uncertain what’s causing your rash, a board-certified dermatologist can help. To find out how, see Contact dermatitis: Diagnosis and treatment.
Until you see a dermatologist, you may be able to get an idea of what’s causing your rash by going to, Itchy rash could be contact dermatitis. - Stop scratching. The rash can be itchy, but scratching tends to worsen the rash. Scratching can also lead to an infection.
- Relieve the itch with cool compresses, anti-itch medication, or oatmeal baths. To make a cool compress, run cold water over a clean towel, then apply the cool, damp towel to the area for 10-15 minutes a few times daily.
Other ways to get relief are to apply an anti-itch medication that contains 1% hydrocortisone to your rash, slather calamine lotion on your itchy skin, or soak in a cool oatmeal bath. You can buy all these without a prescription.
Calamine lotion and oatmeal baths can also help dry oozing skin. - Apply a fragrance-free moisturizer or barrier repair cream after washing. This helps seal in moisture, which your skin needs. Of course, you want to test this product before applying it widely. When you find a product that won’t cause a skin reaction, apply the moisturizer or barrier repair cream while your skin is still damp after washing. To get the best results, it helps to apply your moisturizer (or barrier repair cream) throughout the day when your skin feels dry.
- Wash new clothes before you wear them. Washing new clothes helps to remove chemical residues and dyes that could cause a reaction.
- Remember two key facts about contact dermatitis. If you suddenly develop a new rash, you can miss a likely cause, unless you know the following:
- The rash may not be caused by what’s touching your skin when you first see the rash. Something that touched your skin hours or days ago may be the cause. A rash from an antibiotic ointment may show up 4 days later.
- You can develop an allergic reaction to a product that you’ve used for years. This can happen for one of two reasons. If the product has been reformulated, it can contain different ingredients. The second reason is that you’ve developed a new allergic reaction.
- Get your skin care advice from your dermatologist. If you have raw, irritated skin or have a skin hypersensitivity, your skin needs special care. Dermatologists are the medical doctors who specialize in skin care. A dermatologist can tell you which products would be best for you and which ones to avoid.
How dermatologists help people who have contact dermatitis
Contact dermatitis can affect your life. A rash can come and go unexpectedly, making it difficult to do your job or enjoy life to the fullest. By teaming up with a dermatologist you can get treatment, often find out what causes your rash, and feel more comfortable.
ITCHY RASH COULD BE CONTACT DERMATITIS
So many things that touch our skin can irritate it or cause an allergic reaction, leading to an itchy and sometimes painful rash. When this happens, you have contact dermatitis.
If you can find and avoid the cause, you can get rid of this rash. Easy as that sounds, discovering the cause can be difficult – but not always. By taking time to think about what touches your skin, you may find the cause on your own. When this is not successful, a dermatologist can help identify the cause.
This dermatologist insight tells you what to look for — and the first question you need to ask yourself.
Where does the rash appear?
The answer to this question often provides your biggest clue. Here are some likely causes, sorted out by where the rash appears.
Around your eyes
Skin around the eyes is thin and delicate, which makes it easier for contact dermatitis to develop there.
Clues to look for: Everything from skin care products that remain on the skin for hours, like an anti-aging cream, to something that touches your skin for seconds, think tweezers and facial cleanser, can cause contact dermatitis in this area.
Here are some possible causes of contact dermatitis in this area:
- Skin care product, makeup, makeup sponge, or makeup remover: Have you started using a new product? If this product touches the skin around your eyes, your skin may be reacting to a fragrance or other ingredient.
If you think one of these could be causing your rash, stop using the product that you think is causing the rash. If your rash clears, you’ve likely found the cause. Switching to a hypoallergenic product may prevent a new rash. - Tweezers, eyelash curler, doorknob, or keys: These items usually contain metal, which can cause an allergic skin reaction. The metal in a doorknob or keys can cause a reaction without directly touching the skin around your eyes. If you grab a doorknob or keys and then rub your eyes, you can transfer metal particles too small to see from your hand to the skin around your eyes.
To find out if metal is causing your rash, stop using metal products like tweezers around your eyes. Stop rubbing your eyes. If the rash goes away, you may have a metal allergy. - Nail polish or artificial nails: If you wear nail polish or artificial nails, try to stop touching the skin around your eyes. If the rash clears, you likely have an allergy to an ingredient in one of these nail products.
An itchy rash around your eyes could be contact dermatitis
If you have contact dermatitis in this area, you may have an allergy to fragrance or nickel.

Side of your face
If you have a rash on the side of your face, you may have developed an allergic reaction to something in your cell phone, shampoo, or one of many other products.
Clues to look for: Think about everything that touches the side of your face, from cell phones to shampoo that briefly runs down it. Then try the following to see if the rash clears when you avoid what you think is causing the rash.
Here are top tips that dermatologists give their patients:
- Cell phone: Stop holding the phone against your face. Use the speakerphone or headphones that have a microphone. If the rash starts to clear, you may be hypersensitive to nickel or cobalt.
- Shampoo or conditioner: When rinsing off shampoo and conditioner, make sure they don’t run down your face or other area of your body. If the rash starts to clear, you may have an allergy to an ingredient, such as fragrance. To avoid another flare-up, try using hypoallergenic hair care products.
- Hair color or perming solution: Wear your hair away from your face. If the rash starts to clear, you may have an allergy to an ingredient in the dye or perming solution.
Cell phones are a common cause of contact dermatitis
Some cell phones contain nickel, which can cause an allergic reaction on your skin.

Lips
An itchy and painful rash on (or around) your lips, along with uncomfortably dry and flaky lips that sometimes split, are signs of contact dermatitis.
Clues to look for: Anything that touches your lips can cause contact dermatitis. The list of possible causes includes musical instruments that touch your lips, lipstick, lip balm, and lip gloss. Here’s how to spot one of these causes:
- Musical instrument: If you play a wind instrument, stop playing it until your rash clears. When that’s not possible, switch to a plastic mouthpiece or try a different reed.
- Lip products: Stop applying everything to your lips. If the rash clears, start adding one product a week. If you develop a rash within 7 days of using that product, you’ve likely found the cause.
Musical instruments are a common cause of contact dermatitis
Many musicians who play a wind instrument develop an allergy to metal in the mouthpiece.

Lips and one hand
Clue to look for: The best way to figure out if contact dermatitis is causing this rash is to stop using e-cigarettes. If the rash clears, you’ve likely found the cause.
E-cigarettes often contain nickel, which can cause contact dermatitis
If you have a rash on your lips and the hand that you hold your e-cigarette with, you may have contact dermatitis.

Skin beneath jewelry or glasses
Jewelry and eyeglass frames can contain metals known to cause an allergic skin reaction. Even plastic frames on eyeglasses or sunglasses can cause a reaction.
Clues to look for: If you have an itchy or painful rash beneath a piece of jewelry or where glasses touch your skin, dermatologists recommend the following:
- Jewelry: When a rash develops beneath a ring, necklace, watch, or other piece of jewelry, stop wearing the jewelry. If the rash clears, start wearing that piece again. If the rash returns, you may have an allergy to a metal like nickel, brass, palladium, gold, or silver.
- Eyeglasses or sunglasses: If you wear eyeglasses or sunglasses and develop a rash near or around your ears, you may have developed an allergy to a metal in the frames. A frame that contains nickel, palladium, or titanium can cause an allergic reaction.
Some people’s skin reacts to a plasticizer, UV stabilizer, or varnish used to make the glasses. If you can, wear contact lenses instead of glasses for a while. If the rash clears, it may be time to switch frames. Some frames are hypoallergenic.
Tip dermatologists give their patients: If you have a rash beneath a ring, soap and water may be irritating the skin beneath. You may be able to get rid of the rash by removing your ring before you wash your hands. Before putting your ring back on, dry your hands thoroughly.
Jewelry is a common cause of contact dermatitis
A rash can develop beneath a new piece of jewelry or one you’ve worn for 20 years.

Legs
If you have a rash on one or both legs, you may have developed an allergic reaction to clothing dye, fragrance in your moisturizer, or poison ivy.
Clues to look for: Try to avoid what you think is causing the rash.
- Clothing: Dyes, metals, and fabrics can cause contact dermatitis anywhere on your body, including your legs. Some people wear certain clothing for years before it causes a problem. For example, if you’ve been wearing black pants for years but start having a rash on your legs, switch to a light color. Skip black and red pants. If the rash diminishes or clears, you may have found the cause – the dye.
If you have a rash on your legs, you also want to avoid rough-feeling fabrics like wool and synthetics like polyester and rayon. These can irritate sensitive skin. Some people develop an allergy to the formaldehyde used in some synthetic fabrics.
If you’ve had contact dermatitis in the past, wash new clothes before wearing them to avoid irritation. - Fragrance: This is one of the most common causes of contact dermatitis. A fragrance in skin care products, foods, and elsewhere can cause everything from a painful itchy rash to hives. If a product you apply to your skin contains fragrance, switch to a product labeled “fragrance free.”
- Plant: If your skin brushes up against certain plants, you can develop a rash. You’ll find a list of plants that can make you itch, along with a map that shows you where they grow in the United States and tips to avoid a rash, at Plants that make you itch.
Tip dermatologists give their patients: To avoid fragrance, use products labeled “fragrance free.” If you see “unscented” on the label, it means the fragrance in a product has been covered up. A fragrance that’s been covered up can still cause an allergic reaction.
Many people develop a rash when their skin touches poison ivy, oak, or sumac
These plants are a common cause of contact dermatitis.
Feet
On the feet, shoes and socks have become a common cause of contact dermatitis. It’s so common that there’s a medical term to describe it — footwear dermatitis.
Clues to look for: If you think that something which touches your feet is causing a reaction, here’s what may be happening.
- Shoes or socks: Materials used to make these include leather, rubber, plastic, fabrics, dyes, metal, and glue. If you develop a hypersensitivity to any of these, you can develop an itchy rash. This rash can develop when you wear a new pair of shoes or put on clean socks that you’ve worn before. If you can, stop wearing the shoes and socks that you had on when you noticed the rash. If the rash disappears, you may have found the cause.
- Foot cream, scrubs, nail polish: Many ingredients in these products, including fragrance, can cause a hypersensitivity. If you’re using one of these products, stop using it and see if the rash clears. When using two or more of these products, stop using all of them. Then, add the products back into your routine one at a time. Use one product for a week before adding the next one. This can help you see what’s causing the rash.
- Medications, powders, and deodorants you apply to your feet: Some people develop an allergy to an antibiotic that they apply to their skin like neomycin. A fragrance in a foot powder or deodorant can also trigger contact dermatitis. If you’re using a prescription medication, tell the doctor who prescribed it what’s happening.
Itchy feet can be a symptom of contact dermatitis
Unlike itchy athlete’s foot, contact dermatitis often affects only on the tops of the feet.

When to see a dermatologist
If you cannot get rid of the itchy rash or it returns, it’s time to see a board-certified dermatologist. With more than 15,000 allergens, it can be difficult to find what’s causing a rash.
There are tests that can help a dermatologist find out what is causing your rash. It’s also possible that you have another skin condition. To effectively treat your skin, you need to know what’s causing your rash.
Alopecia Areata
Alopecia areata is an autoimmune disease in which the body's own immune system mistakenly attacks the hair follicles from which hair grows. In most cases, the hair falls out in small, round patches about the size of a quarter. In rare cases, alopecia areata can cause more extensive hair loss on the head, face, and body. The impact on a person's appearance can be a source of emotional stress.
Genetics may predispose some people to the disease. Alopecia areata affects people of all ages and ethnic backgrounds and often begins in childhood. The cause of alopecia areata is unknown, but a trigger, such as a virus or something in the environment, may cause the immune system to attack the hair follicles. The follicles shrink and hair production ceases. However, it's possible for the hair to regrow, as the stem cells that supply the follicle with new hair-growing cells do not seem to be targeted.
The course of alopecia areata is unpredictable and there is no known prevention. Small patches of hair loss usually regrow within one year. More extensive hair loss may take longer to regrow. Some people with alopecia areata have persistent hair loss, or have repeated episodes of hair loss. It is a good idea to keep hairless patches covered with sunscreen and sun-protective clothing (scarves, sunglasses, hats).
There is neither a cure for alopecia areata nor drugs approved for its treatment. However, there are treatments that can help stimulate hair growth, though they don't prevent the appearance of new patches.
Common treatments include:
- Corticosteroids (injections, oral, topical)
- Rogaine (minoxidil) applied topically
- Systemic immune-modulating agents, such as sulfasalazine
Basal Cell Carcinoma
Basal cell carcinoma is the most common type of skin cancer, accounting for 80% of all skin cancers. Basal cell carcinoma most often appears on areas of the body that have the greatest amount of sun exposure. This includes the face, ears, scalp, back of the neck, and back of the arms and hands.
There are three subtypes of basal cell carcinoma:
- Superficial basal cell carcinoma appears as a reddish spot or patch with a fine scale on the top, sometimes with a small erosion on the surface.
- Nodular basal cell carcinoma appears as a waxy or translucent nodule with a pearly white or brown pigmentation, and possibly fine blood vessels (capillaries) on its surface
- Sclerosing (or morpheaform) basal cell carcinoma appears like a scar with poorly defined, blurred borders. It is usually flat with a thinning of the skin.
- A sore that comes and goes but never completely heals or bleeds.
- A shiny bump or nodule, especially if it appears pearly or translucent or brown/reddish like a mole
- A slightly raised pink growth with a crusted depression in the center, possibly with tiny blood vessels visible on the surface
- A patch of skin that is red or irritated, especially on the chest, shoulders, arms or legs
- A white or yellowish waxy scar with poorly defined borders
Your doctor will recommend a treatment based on your medical history and the type of basal cell carcinoma, its size, shape, and location. Treatment options include medications such as 5-fluorouracil and imiquimod cream, curettage & desiccation, cryotherapy, excision, and Mohs surgery. The best treatment is early detection.
Cysts
Cysts are harmless growths in the deeper layers of the skin. They are small closed sacs containing fluid or solid material composed of dead skin cells. There are many types of cysts of different sizes that appear on various parts of the body. Ruptured cysts can become inflamed (red and painful) and discharge pus. Occasionally cysts become infected and resemble a boil. Cysts may require minor surgery to be removed.
Cysts may form when the lining of a hair follicle gets blocked. The cyst sac is filled with a whitish material that can sometimes ooze out onto the skin's surface (most commonly when the cyst is manipulated or traumatized). It is not known why cysts appear or why some people are more prone to get them than others.
Small cysts usually don't need treatment, but can be removed. Larger cysts are usually surgically removed to avoid problems with inflammation and infection or for cosmetic appearance.
Cysts are treated by making a surgical opening in the skin and removing the sac (excision). This is done under local anesthetic and may require stitches. Cysts may recur and need further treatment. If the cyst is inflamed or infected, antibiotics may be prescribed.
Dandruff (Seborrhea)
Dandruff is the shedding of excessive amounts of dead skin from the scalp. Dandruff usually leads to some degree of scalp itching, but sometimes there is no redness or other skin abnormalities. The cause of dandruff is unknown, but may be related to the overgrowth of certain yeasts on the scalp. The yeasts grow on the skin of nearly everyone, but some people are susceptible to an overgrowth that can lead to itching and dry, flaky skin.
Dandruff often shows up as white flakes on dark clothing. Severe dandruff may be due to seborrheic dermatitis. This may be suspected if the scalp is red, or there is greasy scaling on the scalp, behind the ears, or on the face (eyebrows, sides of the nose).
There is no known prevention for the condition. Dandruff usually worsens in dry, winter weather and improves in warm, humid conditions. Dandruff may also worsen during times of stress.
Dandruff cannot be cured, but it can be controlled with regular hair washing, particularly with medicated shampoos. Effective dandruff shampoos might include the following ingredients: selenium sulfide (Selsun Blue), zinc pyrithione (Head & Shoulders, ZNP), ketoconazole (Nizoral AD), tar (T/Gel, Pentrax) or sulfur (Sebulex). Seborrheic dermatitis is a related condition that can be controlled with prescription medications, including prescription-strength shampoos.
Dermatofibroma
Dermatofibromas are firm bumps, or nodules, that form in the deep layers of the skin. Dermatofibromas are harmless and common. They tend to occur in response to an injury, such as an insect bite or ingrown hair. This makes them more likely to appear on the arms and legs. Dermatofibromas may persist indefinitely.
They can appear pink or a dull red, or can resemble a mole (nevus). They are usually small (about a quarter- to a half-inch wide) but can grow to be over an inch in diameter. When pinched, dermatofibromas tend to create a dimple on the skin where the nodule attaches to the upper layers of the skin.
There is no prevention dermatofibromas, especially if the skin responds to injury by producing a dermatofibroma.
Dermatofibromas are benign lesions that do not require treatment. If they are painful or their presence is bothersome (for example - easily traumatized by shaving) they can be removed with surgery.
Dry Skin
Dry skin (xerosis), is often itchy and irritating. Dry skin results from the loss of oils (sebum) in the skin that serve as a natural moisturizer. The tendency for dry skin runs in families and is usually a recurring problem, especially in winter. Because of this seasonal occurrence, it is sometimes referred to as “winter itch".
Dry skin may occur with excessive bathing (particularly with hot water), low humidity (in desert climates or cold winter weather), advancing age, or the use of drying soaps (antibacterial and deodorant soaps).
It is important to regularly apply a moisturizer when your skin becomes dry. Moisturizer is best applied within 3 minutes after a shower or bath when your skin is still damp, but not wet.
Use hypoallergenic and fragrance-free moisturizers. The drier the skin, the “thicker” the moisturizer should be (in order of increasing "thickness" - lotions, creams, ointments). For some people with very dry skin, petrolatum (Vaseline) is quickly absorbed and may be required to sufficiently moisturize the skin. Other effective moisturizers that are readily available include: CeraVe, Cetaphil, and Eucerin creams and Aquaphor. In severe cases, your doctor may recommend a urea- or lactic-acid based product.
Eczema (Dermatitis)
Eczema (dermatitis) is an itchy rash with inflamed skin. Symptoms can range in severity from mild itching and redness to severe blistering and cracked skin. Acute eczema can be red, blistering, or oozing. Chronic eczema can be thickened, rough, and darker than the surrounding skin due to prolonged scratching. Almost always, eczema itches.
Atopic dermatitis, the most common form of eczema, causes dry, sensitive skin. It often appears in infants and toddlers who may “grow out of it” by school age. Contact dermatitis, another common type of eczema, is a localized skin reaction to an allergen or irritant, causing redness, inflammation, and intense itching. Other types of eczema appear on the lower legs (nummular or xerotic eczema), on the palms and soles as small itchy blisters (dyshidrotic eczema), or on the scalp.
Avoid irritants, such as harsh soaps, hot water, detergents, and fragranced products. Moisturize with thick cream or ointment after bathing. Children and young adults often outgrow atopic dermatitis.
Regular treatment can bring relief and may also reduce the severity and duration of eczema. External medications such as cortisone creams, ointments, or lotions can be prescribed. Internal medications such as antihistamines may help alleviate the itch. Oral antibiotics may be prescribed if there is also a secondary infection. Patch testing is an option for some cases of contact dermatitis. For severe cases, ultraviolet light (UVL) treatment may be recommended.
Melanoma
Melanoma is the most serious type of skin cancer because it has a tendency to spread quickly to other parts of the body (metastasize). Most melanomas appear as dark growths similar to moles, but some may be pink, red, or skin-colored. Melanoma is very treatable when detected early, but can be fatal if allowed to spread throughout the body. The goal is to detect melanoma early, when it is still on the surface of the skin.
Sometimes the first sign of melanoma is a change in the size, shape, color, or feel of an existing mole. Most melanomas have a black or blue-black area. Melanoma also may appear as a new mole. It may be black, abnormal, or “ugly looking". More advanced melanoma may have a hard or lumpy texture. More advanced tumors may itch, ooze, or bleed, but are usually not painful.
Excessive sun exposure, especially severe blistering sunburns during childhood or use of tanning beds, can cause melanoma. Early detection and treatment are critical to a successful recovery. Monthly self-exams are important for anyone at risk for developing skin cancer.
Watch for these changes in moles and report them to your doctor:
- Asymmetry with one half of a mole a different shape than the other half
- Border edge is ragged, notched or blurred
- Color is uneven with a variety of hues in the same mole, with areas of black, brown, tan, white, grey, red, pink or blue
- Diameter increases to a size larger than the eraser of a pencil (1/4-inch)
The best treatment is early detection! Your doctor will recommend a treatment based on your medical history and the depth and location of the melanoma. Depending on the size of the tumor, a referral to a surgeon who specializes in cancer surgery may be recommended.
Melanoma Facts
- The incidence of many common cancers is falling, but the incidence of melanoma continues to rise significantly, at a rate faster than that of any of the seven most common cancers.
- Melanoma accounts for about 3% of skin cancer cases, but it causes more than 75% of skin cancer deaths
- Melanoma mortality increased by about 33% from 1975–90, but has remained relatively stable since 1990
- Survival with melanoma increased from 49% between 1950 and 1954 to 92% between 1996 and 2003.
- More than 20 Americans die each day from skin cancer, primarily melanoma. One person dies of melanoma almost every hour (every 62 minutes).
- The survival rate for patients whose melanoma is detected early, before the tumor has penetrated the epidermis, is about 99%. The survival rate falls to 15% for those with advanced disease
- Melanoma is the fifth most common cancer for males and sixth most common for females.
- Women aged 39 and under have a higher probability of developing melanoma than any other cancer except breast cancer.
- Melanoma is the most common form of cancer for young adults 25-29 years old and the second most common form of cancer for adolescents and young adults 15-29 years old.
- About 65% of melanoma cases can be attributed to ultraviolet (UV) radiation from the sun.
- One in 55 people will be diagnosed with melanoma during their lifetime.
- One blistering sunburn in childhood or adolescence more than doubles a person's chances of developing melanoma later in life.
- A person's risk for melanoma doubles if he or she has had five or more sunburns at any age.
Melasma
Melasma is a common skin problem. The condition causes dark, discolored patches on your skin.
It’s also called chloasma, or the “mask of pregnancy,” when it occurs in pregnant women. The condition is much more common in women than men, though men can get it too. According to the American Academy of Dermatology, 90% of people who develop melasma are women.
Melasma causes patches of discoloration. The patches are darker than your usual skin color. It typically occurs on the face and is symmetrical, with matching marks on both sides of the face. Other areas of your body that are often exposed to sun can also develop melasma.
Brownish colored patches usually appear on the
- cheeks
- forehead
- bridge of the nose
- chin
It can also occur on the neck and forearms. The skin discoloration doesn’t do any physical harm, but you may feel self-conscious about the way it looks.
It isn’t totally clear what causes melasma. Darker-skinned individuals are more at risk than those with fair skin. Estrogen and progesterone sensitivity are also associated with the condition. This means birth control pills, pregnancy, and hormone therapy can all trigger melasma. Stress and thyroid disease are also thought to be causes of melasma. Additionally, sun exposure can cause melasma because ultraviolet rays affect the cells that control pigment (melanocytes).
Moles
Moles are very common. Most people have between 10 and 40 moles on their body. They may be pink, tan, brown, or a color similar the person’s normal skin tone. Moles can be flat or raised.
Moles are usually round or oval and smaller than a pencil eraser. They may be present at birth or may appear later on—usually before age 40. People who have dark skin tend to have dark moles. Moles may darken during pregnancy or after sun exposure. Moles tend to fade away in older people.
Avoid sun exposure and use a sunscreen regularly to help prevent moles from developing. Everyone should perform a monthly skin self-exam. This is particularly important if you have many moles on your body. Make an appointment to see your doctor if you notice a new mole, a change in the size, shape or color of a mole, or find another suspicious skin lesion.
Most moles are harmless and do not require treatment. When moles are surgically excised, they normally do not return.
Molluscum Contagiosum
Molluscum contagiosum is a common non-cancerous skin growth caused by a viral infection in the top layers of the skin. They are similar to warts, but are caused by a different virus. The virus is easily spread by skin contact.
Molluscum are usually small, flesh-colored or pink, dome-shaped growths. They may appear shiny and have a small indentation in the center. They are usually found in clusters on the skin of the chest, abdomen, arms, groin, or buttock. They can also involve the face and eyelids.
The molluscum virus is transmitted from the skin of one person who has these growths to the skin of another person, especially where skin-to-skin contact is frequent.
Molluscum can also be sexually transmitted if growths are present in the genital area.
Many dermatologists advise treating molluscum because they spread. They can be frozen with liquid nitrogen or destroyed with various acids, blistering solutions, electrocautery, or a curette. There are also a variety of compounds that can be applied at home. If there are many growths, multiple treatment sessions may be needed to completely clear the lesions.
Nail Fungus (Onychomycosis)
Fungal infection of the toenails and fingernails is referred to as onychomycosis. Toenails are the most vulnerable to fungal infection because they are often injured by repeated trauma in shoes, which creates a space between the nail and nail bed that is hospitable to fungi. If left untreated, onychomycosis can lead to permanent nail damage.
Onychomycosis appears as white or yellowed nails that may be thickened and brittle. One or more nails may be involved, and different parts of a nail may be affected.
Practice good hygiene by keeping hands and feet clean and nails trimmed. Keep your skin dry, especially between the toes. Wear shower sandals in damp public places. Wear well-ventilated shoes, and change socks regularly, especially after exercise. Wear rubber gloves when washing dishes. Sterilize nail clippers and any instruments used in manicures or pedicures.
Onychomycosis is difficult to treat, and recurrence is common. Most antifungal creams and ointments are not every effective because they cannot penetrate the hard nail in sufficient concentration to kill the fungi. There are, however, some formulations specifically designed to penetrate the nail. If the fungal infection has already reached the nail bed, oral antifungal medications may be prescribed. These can reach the nail bed through the blood. If a nail is badly damaged, nail removal may be recommended.
Pre-Cancer (Actinic Keratoses)
Actinic keratoses can be the first step in developing skin cancer. They are common lesions of the epidermis (outermost layer of the skin), and are caused by exposure to sunlight. The most significant predisposing factors for developing AKs is fair skin and long-term sun exposure.
Typical actinic keratoses are dry, scaly, and rough. They are usually pink, but can be skin-colored or tan. They can occur as isolated lesions, but more often are numerous. They are usually found on highly sun-exposed areas such as the face, ears, chest, arms, and lower legs.
You should begin early in life by protecting your skin against sun damage. However, it is never too late to initiate sun protection practices that can aid in prevention of new actinic keratosis lesions in adulthood.
The basic types of treatment for actinic keratoses are cryotherapy, surgical removal and biopsy, topical chemotherapy, and photodynamic therapy.
Psoriasis
Psoriasis is a chronic skin disorder that causes red, scaly patches on the limbs, trunk, scalp, and other parts of the body. It is not contagious. The rash of psoriasis goes through cycles of improving and worsening. A period of worsening is called a "flare". Psoriasis can occur in members of the same family, as there are specific genetic factors that make some individuals more susceptible to psoriasis.
Psoriasis appears as red, thickened areas with silvery scales, most often on the scalp, elbows, knees, legs, arms, genitals, nails, palms, and lower back. It can be itchy or uncomfortable. The skin cells multiply more quickly and accumulate on the surface in silvery scales. Psoriasis comes in many forms. Each differs in severity, duration, location, shape, and pattern of the scales. The most common form, called plaque psoriasis, begins with little red bumps. They can become larger, raised, red patches that flake. Some people with skin psoriasis also have joint pain.
Identify and control triggers (such as stress, certain medications, alcohol, and smoking) and take care of your skin with plenty of moisturizer. Avoid picking and scratching at the skin. Flare-ups sometimes occur in the winter, as a result of dry skin and lack of sunlight. Moisturizing creams and lotions loosen scales and help control itching.
Although there is currently no cure for psoriasis, there are multiple treatments available that can usually lead to a clearing of symptoms. Your doctor may prescribe medications to apply on the skin containing cortisone compounds, synthetic vitamin D analogues, retinoids (vitamin A derivative), tar, or anthralin. Other types of treatment include coal tar, Goeckerman treatment, light therapy, ultraviolet light B (UVB), PUVA, Excimer laser, methotrexate, cyclosporine, and biologic agents.
Rosacea
Rosacea is a chronic skin condition that causes redness and pimples on the face. It can also cause eye irritation. Rosacea occurs most commonly in people 30 to 50 years of age. Although women have rosacea more commonly than men, men tend to suffer more severe forms. Although the cause of rosacea remains unknown, it appears to involve a combination of genetics and environmental factors. It is not contagious.
Rosacea usually develops over a long period of time and progresses to include one or more of the following:
- Facial redness - flushing and persistent redness with visible blood vessels
- Bumps and pus-filled pimples - persistent facial redness with bumps or pimples, inflamed and itchy
- Skin thickening - skin thickening and enlargement, usually around the nose
- Eye irritation - watery or bloodshot eyes, irritation, burning or stinging
Many people report that their rosacea flares up following exposure to certain triggers. Some common rosacea triggers include sun exposure, spicy foods, caffeine, hot baths, alcohol consumption, and emotional stress. Early diagnosis and treatment of rosacea can't prevent it, but can control symptoms, alleviate discomfort, and stop rosacea from progressing.
With treatment and lifestyle modifications, rosacea can be effectively controlled. Rosacea treatments include oral and topical medications (such as doxycycline and Metrogel), lifestyle modifications, and laser and light therapies. Your doctor will recommend a combination of treatments based on the severity and type of rosacea, your skin type, and results from previous treatments.
Scabies
Scabies is a highly contagious skin disease caused by a mite too small to see with the naked eye. The mite burrows just beneath the outer layer of skin and causes itching.
Some people have a widespread, red scaly rash, and others have almost no visible sign of infection. The most common symptom is a rash that itches intensely, especially at night. The rash can be anywhere on your body but is usually on the hands, breasts, genital area, and waistline.
A topical prescription medication is most commonly used to treat scabies. Proper application, along with washing clothing, towels, and bed linens in hot water, kills the mites. Itching and a rash often persist up to 3 weeks following treatment. One treatment usually cures the condition, and most people are no longer contagious. Your doctor may ask you to re-treat yourself after one week.
Seborrheic Keratosis
Seborrheic keratoses are skin growths that appear in adulthood. They can be waxy-looking and covered with a dark crust. Although they may be large and grow quickly, they are benign.
Seborrheic keratoses usually appear as slightly raised, light brown spots and evolve into darker, thicker lesions with rough, warty surfaces. If the growths become unsightly, itch, or become irritated from rubbing against clothing, they can be removed.
Seborrheic keratoses tend to run in families, and there are no known ways to prevent them. They are not caused by sun damage, so they may be found on areas both covered and uncovered by clothing. Because of their appearance, seborrheic keratoses can be confused with other skin growths, such as warts, moles, pre-cancer actinic keratoses, or melanoma.
Seborrheic keratoses are harmless. If treatment is desired, they can be removed. Removal methods most often involve cryotherapy or shave removal.
Shingles
Shingles, also called herpes zoster, is a painful skin rash caused by the same virus that causes chickenpox. After a person recovers from chickenpox, the virus stays in the body. Usually the virus does not cause any problems. However, the virus can reappear years later, causing red patches of tiny blisters to break out on the skin.
Before the rash develops, there is often pain, itching, or tingling in a localized area on one side of the body. In the same area, small blisters and redness develop. The blisters scab after about 5 days. Occasionally, there is also a low grade fever, stomach upset, or headache.
The chickenpox virus (VZV) is present in blisters of shingles. People with shingles can give chickenpox to anyone who has not had chickenpox or has not been vaccinated for chickenpox. Once the rash has developed crusts, the person is no longer contagious.
People with shingles should keep the rash covered, not touch or scratch the rash, and wash their hands often to prevent the spread of VZV.
See your doctor immediately to get on medication that will help shorten the duration and severity of the illness. Several medicines, acyclovir (Zovirax), valacyclovir (Valtrex), and famciclovir (Famyir) are effective at treating shingles. Pain medicine may also help.
Skin Cancer
Most skin cancers develop on the visible outer layer of the skin (the epidermis), particularly on sun-exposed areas like the face, head, hands, arms, and legs. In addition to sun exposure, family history may also play a role. Diagnosing skin cancer usually requires a skin biopsy, where a small piece of skin is removed for examination under a microscope. If skin cancer is detected before it has spread to surrounding tissues, chances of a complete cure are excellent.
Cancer develops when DNA, the molecule found in cells that encodes genetic information, becomes damaged and the body cannot repair the damage. These damaged cells begin to grow and divide uncontrollably. When this occurs in the skin, skin cancer develops. As the damaged cells multiply, they form a tumor. Since skin cancer generally develops in the epidermis, the outermost layers of skin, a tumor is usually clearly visible. This makes most skin cancers detectable in the early stages.
Types of Skin Cancer
Three types of skin cancer account for nearly 100% of all diagnosed cases - basal cell carcinoma, squamous cell carcinoma, and melanoma. Each of these cancers begins in a different type of cell within the skin, and each cancer is named for the type of cell in which it begins.
Skin cancers are divided into one of two classes - nonmelanoma skin cancers and melanoma. Melanoma is the deadliest form of skin cancer.
The most common types of skin cancers are:
- Basal Cell Carcinoma - comes from the basal cells in lowest part of the epidermis. Approximately 80-85% of skin cancers are basal cell carcinomas.
- Squamous Cell Carcinoma - comes from the skin cells (keratinocytes) that make up the top layers of the skin. About 10% of skin cancers are squamous cell carcinoma. Skin cancer may often be preceded by lesions called pre-cancers. The most well-known of these lesions is called actinic keratosis, an early stage of squamous cell carcinoma.
- Melanoma - comes from skin cells called melanocytes, which create pigment called melanin that gives skin its color. Almost 5% of all skin cancers are melanoma. Although less common, melanomas are a very dangerous type of skin cancer and are the leading cause of death from skin cancer.
- All other skin cancers combined account for less than 1% of diagnosed cases. These are classified as nonmelanoma skin cancers and include Merkel cell carcinoma, dermatofibromasarcoma protuberans, Paget's disease, and cutaneous T-cell lymphoma.
- A sore that comes and goes but never completely heals
- A shiny bump or nodule, especially if it appears pearly or translucent (these can look brown or reddish and resemble a mole)
- A slightly raised pink growth with a crusted depression in the center, possibly with tiny blood vessels (capillaries) visible on the surface
- A patch of skin that is red or irritated, especially on the chest, shoulders, or limbs
- A white or yellowish waxy scar with poorly defined borders
Sun protection can significantly decrease a person's risk of developing skin cancer. Sun protection practices include staying out of the sun between 10 a.m. and 4 p.m. when the rays are strongest, applying a broad-spectrum (offers UVA and UVB protection) sunscreen with a Sun Protection Factor (SPF) of 15 or higher year-round to all exposed skin, and wearing a protective clothing, such as a wide-brimmed hat and sunglasses when outdoors.
Since skin cancer is so prevalent today, dermatologists also recommend that everyone learn how to recognize the signs of skin cancer, use this knowledge to perform regular examinations of their skin, and see a dermatologist annually (more frequently if at high risk) for an exam. Skin cancer is highly curable with early detection and proper treatment.
Most skin cancer can be prevented by practicing sun protection, according to numerous research studies. Research also shows that not only does sun protection reduce one's risk of developing skin cancer; sun protection also may decrease the likelihood of recurrence.
Even if you have spent a lot of time in the sun or developed skin cancer, it's never too late to begin protecting your skin. The American Academy of Dermatology (AAD) recommends that everyone protect their skin by following sun protection practices. Several factors determine treatment of skin cancer, including the type, size, extent, location and number of lesions, as well as your medical and family history of skin cancers. Treatment options include: medications such as 5-fluorouracil and imiquimod cream, curettage & desiccation, excision, and Mohs surgery. Radiation and chemotherapy may also be recommended.
Who Gets Skin Cancer?
Skin cancer develops in people of all colors, from the palest to the darkest. However, skin cancer is most likely to occur in those who have fair skin, light-colored eyes, blonde or red hair, a tendency to burn or freckle when exposed to the sun, and a history of sun exposure. Anyone with a family history of skin cancer also has an increased risk of developing skin cancer. In dark-skinned individuals, melanoma most often develops on non-sun-exposed areas, such as the foot, underneath nails, and on the mucous membranes of the mouth, nasal passages, or genitals. Those with fair skin also can have melanoma develop in these areas.
- The majority of people diagnosed with melanoma are white men over age 50.
- 5% of all cancers in men are melanomas; 4% of all cancers in women are melanomas.
- Contrary to popular belief, recent studies show that people receive a fairly consistent dose of ultraviolet radiation over their entire lifetime. Adults over age 40, especially men, have the highest annual exposure to UV.
- Between 1980 and 2004, the annual incidence of melanoma among young women increased by 50%, from 9.4 cases to 13.9 cases per 100,000 women.
- The number of women under age 40 diagnosed with basal cell carcinoma has more than doubled in the last 30 years; the squamous cell carcinoma rate for women has also increased significantly.
- Until age 39, women are almost twice as likely to develop melanoma as men. Starting at age 40, melanoma incidence in men exceeds incidence in women, and this trend becomes more pronounced with each decade.
- One in 41 men and one in 61 women will develop melanoma in their lifetime.
- Melanoma is one of only three cancers with an increasing mortality rate for men.
While Americans now recognize that overexposure to the sun is unhealthy, the fact remains that most do not protect their skin from the sun's harmful rays. As a result, skin cancer is common in the United States. More than 1 million nonmelanoma skin cancers are diagnosed each year, and approximately one person dies from melanoma every hour.
If current trends continue, 1 in 5 Americans will develop skin cancer during their lifetime. Melanoma continues to rise at an alarming rate. In 1930, 1 in 5,000 Americans was likely to develop melanoma during their lifetime. By 2004, this ratio jumped to 1 in 65. Today, melanoma is the second most common cancer in women aged 20 to 29.
Sun exposure is the leading cause of skin cancer. Scientists now know that exposure to the sun's ultraviolet (UV) rays damages DNA in the skin. The body can usually repair this damage before gene mutations occur and cancer develops. When a person's body cannot repair the damaged DNA, which can occur with cumulative sun exposure, cancer develops.
In some cases, skin cancer is an inherited condition. Between 5% and 10% of melanomas develop in people with a family history of melanoma.
Indoor Tanning and Skin Cancer
- Ultraviolet radiation (UVR) is a proven human carcinogen, according to the U.S. Department of Health and Human Services.
- Frequent tanners using new high-pressure sunlamps may receive as much as 12 times the annual UVA dose compared to the dose they receive from sun exposure. Nearly 30 million people tan indoors in the U.S. every year; 2.3 million of them are teens.
- On an average day, more than one million Americans use tanning salons.
- 71% of tanning salon patrons are girls and women aged 16-29.
- First exposure to tanning beds in youth increases melanoma risk by 75%.
- People who use tanning beds are 2.5 times more likely to develop squamous cell carcinoma and 1.5 times more likely to develop basal cell carcinoma.
- The indoor tanning industry has an annual estimated revenue of $5 billion
Skin Cancer Facts
- Skin cancer is the most common form of cancer in the United States. More than one million skin cancers are diagnosed annually.
- Each year there are more new cases of skin cancer than the combined incidence of cancers of the breast, prostate, lung and colon.
- One in five Americans will develop skin cancer in the course of a lifetime.
- Basal cell carcinoma is the most common form of skin cancer; about one million of the cases diagnosed annually are basal cell carcinomas. Basal cell carcinomas are rarely fatal, but can be highly disfiguring.
- Squamous cell carcinoma is the second most common form of skin cancer. More than 250,000 cases are diagnosed each year, resulting in approximately 2,500 deaths.
- Basal cell carcinoma and squamous cell carcinoma are the two major forms of non-melanoma skin cancer. Between 40-50% of Americans who live to age 65 will have one of these skin cancers at least once
- About 90% of non-melanoma skin cancers are associated with exposure to ultraviolet (UV) radiation from the sun. Up to 90% of the visible changes commonly attributed to aging are caused by the sun.
- Contrary to popular belief, 80% of a person's lifetime sun exposure is not acquired before age 18; only about 23% of lifetime exposure occurs by age 18.
Skin Tags
Skin tags are painless, noncancerous growths on the skin. They’re connected to the skin by a small, thin stalk called a peduncle. Skin tags are common in both men and women, especially after age 50. They can appear anywhere on your body, though they’re commonly found in places where your skin folds such as the:
- armpits
- groin
- thighs
- eyelids
- neck
- area under your breasts
Tiny skin tags may rub off on their own. Most skin tags stay attached to your skin. In general, skin tags don’t require treatment. If skin tags hurt or bother you, you may opt to have them removed.
Your doctor may remove your skin tags by:
- Cryotherapy: Freezing the skin tag with liquid nitrogen.
- Surgical removal: Removing the skin tag with scissors or a scalpel.
- Electrosurgery: Burning off the skin tag with high-frequency electrical energy.
- Ligation: Removing the skin tag by tying it off with surgical thread in order to cut off its blood flow.
It’s unclear exactly what causes skin tags. Since they usually show up in skin folds, friction may play a role. Skin tags are made up of blood vessels and collagen surrounded by an outer layer of skin.
According to a 2008 study, the human papillomavirus (HPV) may be a factor in the development of skin tags. The study analyzed 37 skin tags from various sites of the body. Results showed HPV DNA in almost 50% of the skin tags examined.
Insulin resistance, which may lead to type 2 diabetes and prediabetes, may also play a role in the development of skin tags. People with insulin resistance don’t absorb glucose effectively from the bloodstream. According to a 2010 study, the presence of multiple skin tags was associated with insulin resistance, a high body mass index, and high triglycerides.
Skin tags are also a common side effect of pregnancy. This may be due to pregnancy hormones and weight gain. In rare cases, multiple skin tags can be a sign of a hormone imbalance or an endocrine problem.
Skin tags aren’t contagious. There may be a genetic connection. It isn’t unusual for multiple family members to have them.
How to identify a skin tag
The main way to identify a skin tag is by the peduncle. Unlike moles and some other skin growths, skin tags hang off the skin by this small stalk.
Most skin tags are tiny, typically smaller than 2 millimeters in size. Some can grow as large as several centimeters. Skin tags are soft to the touch. They may be smooth and round, or they may be wrinkly and asymmetrical. Some skin tags are threadlike and resemble grains of rice.
Skin tags may be flesh-colored. They can also be darker than the surrounding skin due to hyperpigmentation. If a skin tag becomes twisted, it may turn black due to a lack of blood flow.
You may be at greater risk of getting skin tags if you:
- are overweight
- are pregnant
- have family members who have skin tags
- have insulin resistance or type 2 diabetes
- have HPV
Skin tags don’t become skin cancer. Irritation may occur if they rub with clothing, jewelry, or other skin. Shave with caution around skin tags. Shaving off a skin tag won’t cause permanent damage, though it may cause pain and prolonged bleeding.
Squamous Cell Carcinoma
Squamous cell carcinoma is the second most common cancer of the skin, with 250,000 people diagnosed annually in the United States. It is found most commonly where the skin is exposed to the sun, including the scalp, upper rim of the ear, face, lips, and shoulders.
Older people with fair complexions and frequent sun exposure are most likely to be affected. If left untreated, squamous cell carcinoma can destroy much of the tissue surrounding the tumor or spread to the lymph nodes and be fatal.
Squamous cell carcinoma can appear in a number of forms. If your skin shows any of these symptoms, consult your doctor as soon as possible:
- A dry, crusted, scaly patch of skin that is red and swollen at the base
- A sore that won’t heal and/or bleeds
- Crusted skin
- A thickened, crusty patch of skin with a raised border with a pebbly, granular base
Early treatment and detection are essential to a successful recovery. Proper sun protection (staying out of the direct sun, wearing protective clothing and using sunscreen) may help to prevent the development of squamous cell carcinoma.
It is important to detect and treat squamous cell carcinoma early before it spreads to other tissues. Dermatologists use a variety of different surgical treatment options depending on location of the tumor, size of the tumor, microscopic characteristics of the tumor, health of the patient, and other factors. Most treatment options are relatively minor office-based procedures that require only local anesthesia. Surgical excision to remove the entire cancer is the most commonly used treatment option.
Sun Burn / Sun Damage
Sunburn is not due to the heat of the sun, but rather to the ultraviolet (UV) radiation bombarding the cells in the deeper layers of the skin. Sunburns can occur on cloudy days and in the winter. Since we cannot feel the radiation, the symptoms appear only after the cells are damaged and become inflamed. A sunburn may not be apparent until after you have gotten out of the sun. The pain of sunburn also worsens over time, reaching a peak 12 to 48 hours later. Damaged skin later peels off, usually 2 to 7 days later.
Sunburn has long-term risks. Blistering sunburns, particularly in children, increase the risk of melanoma. Ongoing sun exposure, even without burning, leads to premature aging of the skin and skin cancer.Skin is sunburned when it becomes red, warm, and painful after exposure to ultraviolet light from the sun or tanning booths. Moderate cases can lead to temporary disability, and severe cases can lead to swelling, blistering, fever, and dehydration.
Once the skin has burned, there is little that can be done other than providing comfort while the body heals itself. Therefore, prevention is the most important step to take. Use ample, frequently applied sunscreen with a broad-spectrum SPF 30 and above. When outdoors, wear sun-protective clothing, hats, and sunglasses to protect the skin and eyes from harmful UV rays.
If you get a sunburn, taking a cool shower or bath, or placing cold, wet washcloths over the burn will help the symptoms. Over-the-counter medications like ibuprofen or aspirin may help (aspirin should not be given to children with a fever, or to those who are allergic). Avoid using products containing benzocaine or lidocaine, which can further damage the skin, or petrolatum (Vaseline), which can block pores.
Tinea Versicolor
Tinea versicolor is a common skin condition caused by the overgrowth of a type of yeast that is ubiquitous on human skin. The overgrowth causes uneven skin color and scaling that may be mildly itchy and unsightly. Tinea versicolor is not contagious. Pigment changes may last for months after treatment. The condition may come back during the warm months.
When the yeast grows in colonies, it produces a chemical that causes the skin to change color. The spots may appear pink or coppery brown in patients with fair skin. In darker skinned individuals, the spots may appear lighter than the surrounding skin. The rash tends to appear on the upper back, shoulders, and chest, where the yeast thrives. It may also be seen on the limbs and face.
Tinea versicolor may be associated with excessive perspiration. People with tinea versicolor may notice that it comes back or worsens during hot summer months, and becomes more noticeable with sun exposure.
Treatment consists of antifungal medications applied to the skin. These medications include clotrimazole, ketoconazole, miconazole, and terbinifine. Many over-the-counter dandruff shampoos contain antifungal ingredients and can be applied to the skin for 10 minutes each day in the shower to treat the lesions. In cases of persistent tinea versicolor, oral antifungal medications may be recommended.
Vitiligo
Vitiligo is a condition in which white patches appear on the skin. It currently affects 1-2 million Americans of all races and both sexes equally. Most people with vitiligo develop it before their 40th birthday. Vitiligo most commonly appears on areas most exposed to the sun such as the hands, feet, arms, face, eyelids, lips and nostrils, but it can also appear in the armpits and groin.
The cause is not known. Vitiligo may be an autoimmune disease in which the immune system mistakenly attacks the skin's melanocytes that make melanin, the pigment in your skin. If these cells cannot form melanin, the skin becomes completely white.
There is no known way to prevent vitiligo. To minimize the appearance of vitiligo, practice sun protection using sunscreen and protective clothing. For those with light or medium skin color, avoiding tanning can make areas of vitiligo almost unnoticeable. While vitiligo may run in families, most children whose parents have the disorder will not get it.
There are several treatment options for vitiligo aimed at restoring color to the white patches of skin. Some can have unwanted side effects, may take a long time, or may not be effective.
Depending on the extent of the white patches, treatment options include:
- Medical - medicines (such as topical corticosteroids and topical calcineurin inhibitors), Excimer laser, PUVA (combination of medicine with ultraviolet light therapy), and depigmentation therapy (removing the color from other areas to better match the white patches)
- Surgical - skin grafts and tattooing for small areas of skin
- Cosmetic - makeup or dye to cover the white patches
Warts
Warts are growths on the skin caused by the human papillomavirus (HPV). Warts are very common, particularly in school-age children. Warts can spread by direct contact to other parts of the body, or to others. They are usually painless, but are occasionally painful, especially when they appear on the soles of the feet.
There are 3 main types of warts:
- Common warts (verruca vulgaris) can appear anywhere on dry skin, but they are more commonly seen on the hands. They can appear in clusters, known as mosaic warts.
- Flat warts are often located on the face or legs. They are smaller and can be difficult to see. They tend to grow in large numbers, 20-100 at any one time.
- Plantar warts are located on the soles of the feet. These may be painful.
Warts are usually skin-colored and feel rough to the touch, but they can be dark, flat, and smooth. The HPV virus enters the skin through a small scratch or wound. This explains why warts often appear around fingernails where the skin is often dry or cracked. After the skin becomes infected by the HPV virus, skin cells start reproducing more rapidly. This creates small bumps where the skin becomes a bit thicker than the surrounding skin.
Most people who are exposed to the HPV virus do not develop warts. Warts can be passed from person to person, sometimes indirectly. However, the risk of catching hand, foot, or flat warts from another person is small. The time from the first contact to the time warts have grown large enough to be visible is often several months.
Warts tend to heal on their own within a few years, once the body's immune system recognizes the virus as foreign and starts to attack the underlying infection. However, warts can also be removed. Warts have a tendency to return, so repeated treatments may be necessary.
Common treatments include:
- Occlusion—covering the wart in a bandage or strip of tape
- Over the counter medications (salicylic acid)
- Cryotherapy (freezing off)
- Electrosurgery (burning off)
- Prescription medications
- Other treatments for hard to heal cases
How often should I get a skin check?
We recommend that you have a yearly skin check with your dermatologist to detect any suspicious moles or unusual lesions. If you have skin cancer, your doctor will recommend the frequency of your ongoing skin checks. Check your own skin monthly to detect any changes early on.
What happens during a full body skin check?
A complete skin exam is a visual inspection of your skin by a board-certified dermatologist. A gown is provided for privacy. The complete skin exam takes approximately 5 minutes to complete. If no suspicious lesions are found during your exam, yearly skin exams will usually be recommended. If suspicious lesions are found, the physician will typically recommend a biopsy to rule out skin cancer. Biopsies are performed in the office, usually at the time of your skin exam.
What happens during a skin biopsy?
A biopsy is a procedure performed in the doctor's office that removes a portion of skin for diagnostic testing. Skin biopsies are frequently performed on dark spots, moles, or other skin lesions to determine if they may be skin cancer. The tissue is examined under a microscope. The results of the biopsy are provided in a pathology report. It may take 4-10 days to obtain the pathology report.
The type of skin biopsy preformed depends on the suspected cause of the skin lesion and its location on the body. First, the doctor numbs the area of skin to be biopsied with a local anesthetic (lidocaine).
The doctor then removes the lesion in one of the following ways:
- Shave biopsy is performed with either a small scalpel blade or a curved razor blade, The blade removes only a small portion of the lesion leaving the skin primarily intact. Electrocautery may be performed to heat the wound and stop any bleeding. Shave biopsies are frequently performed on lesions suspected to be basal cell carcinoma or squamous cell carcinoma.
- Punch biopsy is performed with a round knife, similar to a very small cookie cutter. Stitches may be required to close the wound, though small punch biopsies may heal without stitches.
- Excisional biopsy is performed with a scalpel. It is used to create an elliptical cut around the lesion and obtain some of the subcutaneous fat below the dermis. An excisional biopsy is frequently performed for lesions suspected to be melanoma. The wound created by an excisional biopsy is usually closed with stitches (sutures).


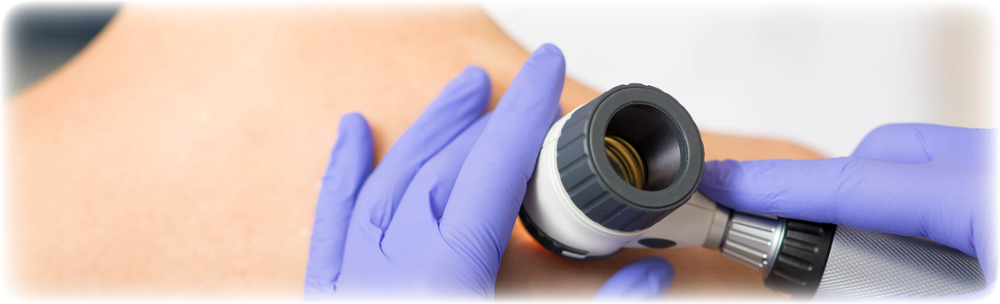

.png?width=850&height=850&name=lane%20badge%20(1).png)


-1.png?width=711&height=711&name=healthy%20br%20(4)-1.png)

