COVID-19 UPDATE – May 11, 2023
On January 31, 2020, the U.S. Department of Health and Human Services (HHS) declared, under Section 319 of the Public Health Service Act, a U.S. public health emergency because of the emergence of a novel virus (a new strain of a virus that has not been seen before). After 13 renewals, the public health emergency expired on May 11, 2023. Although COVID-19 no longer poses the societal emergency that it did when it first emerged late in 2019, COVID-19 remains an ongoing public health challenge.
On April 18, 2023, The U.S. Food and Drug Administration amended the emergency use authorization (EUAs) of the Moderna and Pfizer-BioNTech COVID-19 bivalent mRNA vaccines to simplify the vaccination schedule for most individuals. This action included authorizing the current bivalent vaccines to be used for all doses administered to individuals 6 months of age and older. The monovalent Moderna and Pfizer-BioNTech COVID-19 vaccines are no longer authorized for use in the Unites States and have been removed from the market.
What You Need to Know:
- Most individuals, depending on age, previously vaccinated with a monovalent COVID-19 vaccine who have not yet received a dose of bivalent vaccine may receive a single dose of a bivalent vaccine
- Most individuals who have already received a single dose of the bivalent vaccine are not currently eligible for another dose.
- Individuals 65 years of age and older who have received a single dose of a bivalent vaccine may receive one additional dose at least four months following their initial bivalent dose.
- Most individuals with certain kinds of immunocompromise who have received a bivalent COVID-19 vaccine may receive a single additional dose of a bivalent COVID-19 vaccine at least 2 months following a dose of a bivalent COVID-19 vaccine, and additional doses may be administered at the discretion of, and at intervals determined by, their healthcare provider.
- Most unvaccinated individuals may receive a single dose of a bivalent vaccine, rather than multiple doses of the original monovalent mRNA vaccines.
- Children 6 months through 5 years of age who are unvaccinated may receive a two-dose series of the Moderna bivalent vaccine (6 months through 5 years of age) OR a three-dose series of the Pfizer-BioNTech bivalent vaccine (6 months through 4 years of age). Children who are 5 years of age may receive two doses of the Moderna bivalent vaccine or a single dose of the Pfizer-BioNTech bivalent vaccine.
- Children 6 months through 5 years of age who have received one, two or three doses of a monovalent COVID-19 vaccine may receive a bivalent vaccine, but the number of doses that they receive will depend on the vaccine and their vaccination history.
At this stage of the pandemic, data supports simplifying the use of the authorized MRNA bivalent COVID-19 vaccines and the FDA believes this approach will help encourage future vaccinations. Evidence is now available that most of the U.S, populations 5 years and older has antibodies to SARS-CoV-2, the virus that causes COVID-19, either from vaccination or infection that can serve as a foundation for the protection provided by the bivalent vaccines. COVID-19 continues to be a very real risk for many people, and encourage individuals to consider staying current with vaccination, including a bivalent COVID-19 vaccine. The available data continue to demonstrate that vaccines prevent the most serious outcomes of COVID-19, which are severe illness, hospitalization and death.
Current Covid-19 Vaccines Authorized for Emergency Use or FDA Approved are:
- Pfizer-BioNtech COVID-19 Vaccine, Bivalent
- Moderna COVID-19 Vaccine, Bivalent
- Janssen Covid-19 Vaccine
- Novavax COVID-19 Vaccine, Adjuvanted
February 27, 2022
The American Nurses Association (ANA), American Hospital Association (AHA), and American Medical Association (AMA) encourage everyone to make sure they are up-to-date on their COVID-19 vaccines, including the updated bivalent booster dose when eligible.
COVID-19 Treatments and Medications - January 10, 2022
What You Need to Know
- If you test positive for COVID-19 and are more likely to get very sick, treatments are available that can reduce your chances of hospitalization and death.
- Don’t delay: Treatment must be started within days after you first develop symptoms to be effective.
- Other medications can help reduce symptoms and help you manage your illness.
- The Treatment Locator (hhs.gov) can help you find a location that offers testing and treatment or a pharmacy where you can fill your prescription.
Treating COVID-19

If you test positive and are more likely to get very sick from COVID-19, treatments are available that can reduce your chances of being hospitalized or dying from the disease. Medications to treat COVID-19 must be prescribed by a healthcare provider and started as soon as possible after diagnosis to be effective. Contact a healthcare provider right away to determine if you are eligible for treatment, even if your symptoms are mild right now.
Don’t delay: Treatment must be started within days of when you first develop symptoms to be effective.
People who are more likely to get very sick include older adults (ages 50 years or more, with risk increasing with age), people who are unvaccinated, and people with certain medical conditions, such as chronic lung disease, heart disease, or a weakened immune system. Being vaccinated makes you much less likely to get very sick. Still, some vaccinated people, especially those ages 65 years or older or who have other risk factors for severe disease, may benefit from treatment if they get COVID-19. A healthcare provider will help decide which treatment, if any, is right for you. Check with your healthcare provider or pharmacist if you are taking other medications to make sure the COVID-19 treatments can be safely taken at the same time.
Treatments

The FDA has authorized antiviral medications to treat mild to moderate COVID-19 in people who are more likely to get very sick.
- Antiviral treatmentstarget specific parts of the virus to stop it from multiplying in the body, helping to prevent severe illness and death.
The National Institutes of Health (NIH) provides COVID-19 Treatment Guidelines for healthcare providers to help them work with their patients and determine the best treatment options for them. Several options are available for treating COVID-19. They include:
Nirmatrelvir with Ritonavir (Paxlovid)
Antiviral
Adults; children ages 12 years and older
Start as soon as possible; must begin within 5 days of when symptoms start
Taken at home by mouth (orally)
Remdesivir (Veklury)
Antiviral
Adults and children
Start as soon as possible; must begin within 7 days of when symptoms start
Intravenous (IV) infusions at a healthcare facility for 3 consecutive days
Molnupiravir (Lagevrio)
Antiviral
Adults
Start as soon as possible; must begin within 5 days of when symptoms start
Taken at home by mouth (orally)
Some treatments might have side effects or interact with other medications you are taking. Ask a healthcare provider if medications to treat COVID-19 are right for you. If you don’t have a healthcare provider, visit a Test to Treat location or contact your local community health center or health department.
If you are hospitalized, your healthcare provider might use other types of treatments, depending on how sick you are. These could include medications to treat the virus, reduce an overactive immune response, or treat COVID-19 complications.
Convalescent Plasma
Some people with COVID-19 who are immunocompromised or are receiving immunosuppressive treatment may benefit from a treatment called convalescent plasma. Your healthcare provider can help decide whether this treatment is right for you.
Managing COVID-19 symptoms

Most people with COVID-19 have mild illness and can recover at home. You can treat symptoms with over-the-counter medicines, such as acetaminophen (Tylenol) or ibuprofen (Motrin, Advil), to help you feel better.
Learn more about what to do if you are sick.
Preventing COVID-19
COVID-19 vaccines
COVID-19 vaccines available in the United States effectively protect people from getting seriously ill, being hospitalized, and even dying—especially people who are boosted. As with vaccines for other diseases, you are protected best when you stay up to date. CDC recommends that everyone who is eligible stay up to date on their COVID-19 vaccines.
Preventive medications
The FDA has issued an emergency use authorization for tixagevimab plus cilgavimab (EVUSHELDTM), a medicine that can help protect you from getting COVID-19. EVUSHELDTM contains two different antibodies and is given as two separate consecutive intramuscular (IM) injections at a doctor’s office or healthcare facility before you are exposed or test positive for COVID-19. If you are moderately or severely immunocompromised, or severely allergic to COVID-19 vaccines, you may be eligible for EVUSHELDTM every 6 months. EVUSHELDTM may offer less protection against certain strains of the Omicron variant. It is important that even if you receive EVUSHELDTM you take multiple prevention measures. Additionally, you should undergo testing and seek medical attention if you develop symptoms of COVID-19, and start treatment for COVID-19 as appropriate. Talk to your healthcare provider to determine if EVUSHELDTM is right for you.
The right medications for COVID-19 can help. People have been seriously harmed and even died after taking products not approved for use to treat or prevent COVID-19, even products approved or prescribed for other uses. Talk to a healthcare provider about taking medications to treat COVID-19.
Indoor Mask Mandate – Updated February 8, 2022
Due to a state-wide decline in COVID-19, all vaccinated staff, patients and guests are no longer required to wear a mask while inside any Lane building.
All UNVACCINATED patients and guests must wear a mask at all times, unless eating or drinking.
The safety of our team members, patients, and visitors remains a priority, and we encourage you to socially distance, mask, and get vaccinated and/or your booster dose.
CDC Updates and Shortens Recommended Isolation and Quarantine Period
for General Population - Updated December 30, 2021
Isolation and Quarantine
CDC has updated isolation and quarantine recommendations for the public. These recommendations do not apply to healthcare personnel and do not supersede state, local, tribal, of territorial laws, rules, and regulations.
People with COVID-19 should isolate for 5 days and if they are asymptomatic or their symptoms are resolving (without fever for 24 hours), follow that by 5 days of wearing a mask when around others.
Recommendations for people who are exposed to COVID-19 are also updated. If you are unvaccinated or more than 6 months out from your second mRNA dose (or more than 2 months after the J&J vaccine) and you are not yet boosted, CDC recommends a quarantine for 5 days followed by strict mask use for an additional 5 days. If a 5-day quarantine is not feasible, it is imperative that an exposed person wear a well-fitting mask at all times when around others for 10 days after exposure.
People who have received their booster shot do not need to quarantine following an exposure but should wear a mask for 10 days after the exposure. For all those exposed, best practice would also include a test for COVID-19 at day 5 after exposure. If symptoms occur, individuals should immediately quarantine until a negative test confirms symptoms are not attributable to COVID-19.
Omicron Variant – Updated December 6, 2021
 On November 26, 2021, the World Health Organization classified a new COVID-19 variant as a variant of concern and named it Omicron. As of December 4, 2021, Omicron has been identified in the United States and is reported now in more than 20 countries.
On November 26, 2021, the World Health Organization classified a new COVID-19 variant as a variant of concern and named it Omicron. As of December 4, 2021, Omicron has been identified in the United States and is reported now in more than 20 countries.
CDC has been actively monitoring and preparing for this variant and continues to work diligently with other U.S. and global public health and industry partners to learn more.
The virus that causes COVID-19 is constantly changing, and new variants of the virus are expected to occur. Sometimes new variants emerge and disappear. Other times, new variants persist.
The recent emergence of the Omicron variant further emphasizes the importance of vaccination, boosters, and general prevention strategies needed to protect against COVID-19. Everyone 5 and older should get vaccinated and boosters are recommended for everyone 18 years and older.
Learn more: https://www.cdc.gov/coronavirus/2019-ncov/variants/about-variants.html?ACSTrackingID=USCDC_2067-DM71450&ACSTrackingLabel=Omicron%20Variant%20%20%7C%20COVID-19&deliveryName=USCDC_2067-DM71450
As the new Omicron variant spreads worldwide, the Louisiana Department of Health continues to monitor the situation in our state and strongly recommends that people in Louisiana prepare and take action to protect themselves and their families.
- This is a time to prepare but not panic.
- People who are vaccinated and eligible for a booster need to use this time to get their boosters.
- Those who are not vaccinated should get vaccinated.
- All international travelers, regardless of vaccination status or recent history of COVID-19 infection, should be tested 3-5 days after arrival.
- Now that we are entering the winter holiday season, it’s also more important than ever to use those public health tools we know work – mask according to applicable guidelines, practice good hand hygiene, and get tested and stay home if you feel sick.
KEY FACTS
- Omicron, formally classified by the World Health Organization (WHO) as B.1.1.529, has been detected in at least 30 countries, and there are now three known cases in the United States in California, Colorado and Minnesota as of December 2, 2021.
- The best protection against Omicron is getting fully vaccinated and, if you’re eligible, getting a booster shot.
- All international travelers should be tested 3-5 days after international travel.
- Although new information is emerging, we know that Omicron includes multiple mutations across the SARS-CoV-2 genome.
- This new variant may be more transmissible than previous strains.
- It may carry an increased risk of reinfection compared to other variants of concern.
- Please continue to mask according to applicable CDC guidance, practice good hand hygiene, and get tested and stay home if you feel sick.
- CDC and LDH recommend that everyone ages 5 and older get the COVID-19 vaccine. The vaccines are widely available at more than 1,000 locations in all of Louisiana’s 64 parishes, including at pharmacies, hospitals, healthcare clinics, and doctor’s offices.
- We encourage families to reach out to their local vaccine provider ahead of time to confirm available pediatric vaccines. You can also call 211 or the COVID Vaccine Hotline at 1-855-453-0774 to find a nearby pediatric vaccination location.
- Louisiana's Shot For $100 vaccine incentive program is being extended through the end of the year, giving residents another chance to get their shots throughout the holiday season.
RISK OF COVID TO CHILDREN
- COVID-19 continues to spread throughout Louisiana. Since the beginning of August, 25% of all new COVID-19 cases in Louisiana were in children.
- Our most recent COVID surge was fueled by the highly transmissible Delta variant and had a devastating impact on Louisianans, including children. Tragically, LDH reported 9 pediatric deaths tied to the fourth surge alone. A total of 18 children in Louisiana have died of COVID since the pandemic began.
- At the end of October, about 8,300 American children ages 5 to 11 had been hospitalized with Covid and at least 172 have died according to the Centers for Disease Control and Prevention. Nationally, according to the FDA, at least 94 children ages 5 to 11 have died of COVID-19 since the pandemic began, and 8,300 have become so sick they needed to be hospitalized. In fact, COVID was the eighth-leading cause of death in the age group over the past year, after accidents, cancer, malformations, murder, heart disease, chronic lower respiratory disease, and flu or pneumonia.
- According to the CDC, COVID-19 cases in children can result in hospitalizations, deaths, MIS-C (multi-inflammatory syndrome in children) and long-term complications, such as “long COVID,” in which symptoms can linger for months. The spread of the Delta variant resulted in a surge of COVID-19 cases in children throughout the summer. During a 6-week period in late June to mid-August, COVID-19 hospitalizations among children and adolescents increased fivefold.
- Although, thankfully, we have come down from our fourth and most dangerous surge to date, because of our sub-optimal vaccination rate we remain vulnerable to another, equally devastating surge as with the holiday season upon us.
WHY GET YOUR CHILD VACCINATED
- We know many families have been anxiously awaiting the news that 5-11-year-olds are now eligible, especially following our dangerous fourth surge and as we go into the holiday season.
- Vaccination, along with other preventative measures, can protect children from COVID-19 using the safe and effective vaccines already recommended for use in adolescents and adults in the United States. Similar to what was seen in adult vaccine trials, vaccination was nearly 91 percent effective in preventing COVID-19 among children aged 5-11 years. In clinical trials, vaccine side effects were mild, self-limiting, and similar to those seen in adults and with other vaccines recommended for children. The most common side effect was a sore arm.
- Having your child vaccinated against the virus will help prevent them from getting severe COVID-19 disease. Although COVID-19 in children is often milder than in adults, some children can get severe lung infections, become very sick and need hospital care. The shot makes them stronger and better able to fight off the virus if they come in contact with it.
- The vaccine also helps reduce the spread of COVID-19. Children can transmit the coronavirus to others if they’re infected, even when they have no symptoms. Getting the shot can protect both your child and others, including other children and more vulnerable family members.
- When your child gets vaccinated against COVID-19, they also have a better chance at staying in school and participating in the activities they enjoy.
- With the winter holidays upon us, having the whole family ages 5 & up vaccinated is the best way to ensure a safer holiday season. And if you don't know if your entire gathering is vaccinated, you can always add other precautions - masking, social distancing, getting tested, taking the gathering outside.
- The ability to have your children ages 5 & up vaccinated ensures that your family can enjoy the holidays safely and lowers the risk of transmission of the virus to grandparents, immunocompromised family members, and those who live or work in a high-risk setting.
CALL TO ACTION
- We know parents and families want to make the best decision for their children. And we know that families have questions – that’s good! Talk to your doctor or other healthcare provider today about the shot and to make an appointment. To find a nearby vaccination location, go to www.vaccines.gov, call Louisiana’s COVID-19 Vaccine Hotline at 1-855-453-0774, or visit ldh.la.gov/kidsvax.
- Your child can get the COVID-19 vaccine at the same time they get their annual flu vaccine, if they have not gotten one yet. If your child is behind on other childhood vaccines, they can receive them at the same time as their COVID-19 shot, too.
HOW TO GET A COVID VACCINE IN LOUISIANA
Everyone ages 5 and older is eligible for the COVID-19 vaccine in Louisiana. Parents with children under 18 should confirm with the vaccine provider that the Pfizer vaccine is available before making an appointment.
- COVID-19 vaccines are free and widely available at more than 1,400 locations in all of Louisiana’s 64 parishes, including at pharmacies, hospitals, healthcare clinics, and doctor’s offices.
- For a list of locations, visit LDH’s vaccine directory which can be found at covidvaccine.la.gov or visit vaccines.gov, which is maintained by the federal government.
- To get a list of vaccine locations near you, text your ZIP code to GETVAX (438829) in English, or VACUNA (822862) in Spanish.
- If you have questions, would like to speak with a medical professional, or need help scheduling an appointment, call 211 or Louisiana’s vaccine hotline at 1-855-453-0774.
SHOT FOR 100 INCENTIVE
- The Shot for 100 vaccine incentive program has been extended through December 31. $100 will be given to anyone who gets the first dose of their COVID vaccine at participating community-based vaccination sites around the state. Each individual may only receive the incentive once. More information, including a list of participating sites, is available at shotfor100.com.
- More than 2.5 million Louisianans have already rolled up their sleeves. And while this is welcome news, it's not enough to end this pandemic.
- How to participate:
- There are participating community-based vaccination sites located in every region of the state. You can find them at: shotfor100.com.
- Individuals who choose to go sleeves up at participating sites will be given a deactivated visa card upon vaccination.
Indoor Mask Mandate - Updated November 19, 2021
The Louisiana Department of Health has released health care facilities from the current mandate to be
completely masked while in the facility.
Fully vaccinated individuals (who are not immunocompromised and do not have end stage renal
disease) are now able to be mask-off in general healthcare settings – unless required in specific settings such as when visiting COVID-19 patients.
Unvaccinated persons are required to wear masks at all times, except when eating or drinking.
This new mask-off policy does not impact your choice to remain mask-on.
Visitor Policy – Updated October 9, 2021
As COVID-19 admissions continue to decrease, we are opening all entrances into the hospital for visitors and staff.
Visiting Hours
8 a.m. - 8 p.m.
- Exceptions will be made on a case by case basis.
- All visitors must wear a mask when caregivers enter room or when entering or leaving the building
Safety
With the well-being and protection of our team, patients, and community in mind, we will require all employees, visitors, and patients to adhere to the below safety measures:
- Wear a mask
- Practice social distancing
- Practice consistent hand hygiene
Patient Visitation:
- Inpatient units - Visitation will be allowed during visiting hours with only 1 visitor to stay the night per patient.
- Critical Care Units - 1 visitor will be allowed during designated visiting hours.
- Children Visitors - No children under age 18 unless here for a procedure or end of life visitation.
- Persons Under Investigation (PUI) or confirmed COVID-19 patients -
- 1 visitor, except for end of Overnight guest will be on a case by case basis
- The visitor must wear a mask and remain in the room at all times.
- Vendors - Allowed for direct patient care activities
- Retail Pharmacy/Billing/Medical Records - Visitors allowed during business hours
- Gift Shop - Visitors allowed
- Cafeteria - Visitors allowed
Exceptions to the visitor policy outside of the visiting hours:
- End of Life - A maximum of 2 visitors per room rotating if necessary. Remaining family may wait in waiting areas within the hospital.
- End of life refers to a final period in a person’s life, in which it is medically obvious that death is imminent or a terminal moribund state cannot be prevented.
- Surgery and Procedures - Patients undergoing surgery or being admitted to the hospital may have visitors pre-procedure and if admitted, the visitors must follow the visitation guidelines.
- Outpatient services/Appointment - Patients requiring assistance may have 1 visitor to accompany them during their service/appointment, not limited to visitation hours.
- Emergency Department - 1 visitor will be allowed in the ED, including boarded patients waiting for an inpatient room.
- Labor Delivery/Postpartum - 2 visitors will be allowed and may stay with the patient overnight, not limited to visiting hours
Update 9/2/21 - Regeneron for COVID-19 Treatment
To help reduce hospitalization rates, Lane Regional Medical Center has expanded its Infusion Center to administer monoclonal antibodies to COVID-19 patients who meet treatment criteria.
Located on the 3rd floor of the Lane Medical Plaza and Outpatient Diagnostic Center, at 6550 Main Street in Zachary, the Regeneron Infusion Center is open from 7 a.m. – 7 p.m., seven days a week, and can accommodate administer up to 90 infusions per day. Treatments take between 30 to 50 minutes and require observation of up to an hour afterwards.
Staffing is comprised of Lane team members and additional nursing and medical staff provided by the Louisiana Department of Health.
In 2020, the Food and Drug Administration issued an emergency use authorization allowing monoclonal antibodies as a treatment option for COVID-19. The FDA authorized several different monoclonal antibodies, including Regeneron which is currently being administered at Lane Infusion Center.
A physician referral is required to receive the Regeneron monoclonal antibody treatment at Lane Infusion Center. To be eligible, patients must test positive for COVID-19, have symptoms for 10 days or less, and meet one of the following criteria:
- 65 years old or older
- Have a BMI of more than 25 kg/m2
- Currently pregnant
- Have a medical condition, including:
- Chronic kidney disease
- Cardiovascular disease (including congenital heart disease or hypertension)
- Diabetes
- Down syndrome
- Dementia
- Liver disease
- Chronic lung disease
- Sickle cell disease
- Immunosuppressive disease or receiving immunosuppressive treatment
- Current, or former, smoker
- History of stroke or cerebrovascular disease
- Current, or history of, substance abuse
- Neurodevelopmental disorders or other conditions that confer medical complexity
- Have a medical-related technological dependence (including tracheostomy or gastrostomy)
“The Regeneron infusion treatment is time-sensitive,” says Jason Gwyn, director of Lane Infusion Center. “To get the best results, patients 18 and older should get a physician referral to receive the treatment as soon as possible after testing positive for COVID-19.”
Monoclonal antibodies like Regeneron have proven to be an effective treatment for COVID-19 because once administered, they look for and attach themselves to the spike proteins on the coronavirus that cause COVID-19. Once attached to the spike proteins, these monoclonal antibodies can block the virus’ ability to enter healthy cells, thereby slowing the spread of infection.
For more information, please call Lane Infusion Center at 658-4025.
Symptoms of the COVID-19 Delta Variant
Common symptoms of the COVID-19 Delta Variant can sometimes be mistaken for allergies:
- Sore throat
- Runny nose
- Fever
- Headache
- NOTE: cough and loss of taste and smell are not as common with the Delta variant.
Common symptoms of the original COVID-19 Alpha Variant:
- Fever/chills
- Cough
- Shortness of breath or difficulty breathing
- Fatigue
- Muscle/body aches
- Loss of taste or smell
- Headache
- Sore throat
- Congestion/runny nose
- Nausea/vomiting
- Diarrhea
Masks
The Delta variant is highly contagious, nearly twice as contagious as previous variants. It is currently a state mandate to wear a mask in public indoor places, even if fully vaccinated, to help slow the spread of the virus.
Vaccines
When you get vaccinated, your risk of getting very sick or being hospitalized is significantly lower than someone who has not been vaccinated. At Lane, approximately 90% of our hospitalized COVID-19 patients have not been vaccinated.
When you are ready to get the vaccine, please call Lane Family Practice to schedule an appointment, 225-654-3607.
Visitor Policy – Updated August 11, 2021
Visiting Hours
2 p.m. - 6 p.m. Patient Rooms
No overnight guests allowed.
Visitor Policy - Updated August 4, 2021
As we respond to a new surge of COVID-19, patient and team member safety remain our highest priority.
To ensure the safety of our hospital and community while remaining empathetic to the needs of our patients and families, we will revert back to a single entrance for patients and visitors through the Emergency Department.
- No visitors are allowed in the Emergency Room, except for end of life
- On patient units, non-COVID-19 patients will be allowed a maximum of 1 visitor a day who is allowed to spend the night with the patient if desired. No rotating of visitors will be allowed. Visitor must wear a mask when caregivers enter room or when entering or leaving the room/building.
- On patient units, 1 visitor is allowed to visit patients being treated for COVID-19 during regular visiting hours - No overnight stays and no rotating of visitors will be allowed. Visitor must wear a mask when caregivers enter room or when entering or leaving the room/building. Visitor must remain in the patient’s room at all times, unless exiting the building.
VISITING HOURS
Visiting Hours: 8 a.m. - 6 p.m. Patient Rooms
8 a.m. - 6 p.m. Labor & Delivery / Recovery & Postpartum
SCREENING
All visitors will continue to be screened daily for symptoms, including:
- History of positive COVID-19 diagnosis within the last 10 days
-
Exposure to a positive COVID-19 person within the last 14 days
-
Fever greater than or equal to 100°F
-
Loss of smell/taste
Screeners will be logging and screening visitors entering the facility.
If a visitor says “YES” to any of the screening symptoms or have fever at screening area, they will not be allowed entry into the facility.
SAFETY
With the well-being and protection of our team, patients, and community in mind, we will require all employees, visitors, and patients to adhere to the below safety measures:
- Wear a mask
- Practice social distancing
- Practice consistent hand hygiene
- Visitors must wear a mask when caregivers enter room or when entering or leaving the building
PATIENT VISITATION
Visitors will not be allowed to rotate throughout the day during visitation hours. One visitor may stay overnight with non-COVID-19 patients.
- Inpatient Units: One visitor will be allowed per patient during designated visiting hours.
- Critical Care Units: One visitor will be allowed per patient during designated visiting hours.
- Labor & Delivery: Two visitors are allowed per patient during designated visiting hours.
- Children Visitors: No children under age 18 unless here for a procedure or end of life visitation.
- Persons Under Investigation (PUI) or confirmed COVID-19 patients:
- One visitor, except for end of
- The visitor must wear the recommended personal protective equipment (PPE) for the duration of the visit, including a mask and remain in the room at all times.
- Emergency Department: No visitors are allowed.
- Surgery and Procedures: Patients undergoing surgery or being admitted to the hospital may have 1 designated visitor pre-procedure, and if admitted, visitors must follow the visitation guidelines.
- Outpatient Services/Appointments: Patients may have 1 visitor to accompany them during their service/appointment, not limited to visitation hours.
- Vendors/Referrals: Will be allowed for direct patient care activities.
- Gift shop or Cafeteria: Closed to the general public.
- Retail pharmacy: No customers allowed. Please call 658-6770 to fill a prescription, and a representative will deliver it to you at the ER entrance. Hours 8am-4pm
- Billing: No customers allowed. Please call 844-620-8131 for assistance. To make a payment in person, call 658-4343 and a representative will meet you at the ER entrance.
- Medical Records: No customers allowed. Please call 658-4311 for assistance.
Exceptions to the Visitor Policy outside of Regular Visiting Hours:
- End of Life*: A maximum of 2 visitors per patient, rotating if necessary. Remaining family waiting to see patient will be asked to wait outside or in their vehicle. Clergy will be allowed for end of life situations.
*End of life is defined as anticipated death with an active do-not-resuscitate (DNR) order in place and/or planned withdrawal of life-sustaining interventions (e.g., ventilator).
Update – August 3, 2021
Gov. Edwards Temporarily Reinstates Louisiana's Statewide Mask Mandate as COVID Cases and Hospitalizations Threaten Hospitals' Ability to Serve Communities...
Effective August 2, 2021, Gov. John Bel Edwards has temporarily reinstated Louisiana’s statewide mask mandate indoors for all people age five and older as COVID-19 cases and hospitalizations continue to rise across Louisiana, threatening the ability of Louisiana’s hospitals to deliver care during this fourth surge of COVID. Louisiana is currently in the worst surge of the COVID-19 pandemic so far in terms of case growth rate, percent positivity and hospitalizations.
The Centers for Disease Control and Prevention (CDC) on Friday released data that shows that while vaccination reduces one’s chance of becoming infected with COVID-19, those who do become infected with the Delta variant despite being fully vaccinated are likely at risk of transmitting it to others.
Louisiana’s temporary indoor statewide mask mandate will stay in place until at least September 1, but may be extended if necessary.
Driven largely by Louisiana’s insufficient vaccination rate and the spread of the highly transmissible Delta variant, COVID-19 cases in the state have grown exponentially. Louisiana remains No. 1 nationwide for number of new COVID-19 cases per capita. The temporary indoor statewide mask mandate will help slow the spread of COVID-19 and limit suffering and death in Louisiana until we are through this fourth surge. The indoor mask mandate also applies to K-12 schools, universities, and other higher education institutions, which return to on-campus learning in August. In accordance with new guidance from the CDC, all people on campuses should be masked indoors, regardless of their vaccination status.
“It has never been more clear that we are in an unchecked COVID surge that, in addition to threatening the health and wellbeing of many Louisianans, also threatens the capacity of our hospitals and medical facilities to deliver care to their patients. That is simply unacceptable, and after reviewing new data from the CDC, speaking with public health advisors, and hearing from hospital leadership and the business community, I am reinstating Louisiana’s statewide mask mandate indoors, including in schools to protect our children who are too young to be vaccinated and our teachers and staff,” Gov. Edwards said. “This decision is not one I take lightly, but as the fourth surge of COVID-19 is upon us, we know that mask wearing when you are in public is one way to greatly lower your risk of spreading or catching COVID. Being vaccinated against COVID-19 is another. We have the tools we need to slow the spread of COVID-19 in our communities and save lives, and I am pleading with unvaccinated Louisianans to get their shot as soon as they can to protect themselves. We can end this nightmare, but it is going to take all of us working together to do it.”
“The data in Louisiana clearly point to the severity of our situation, and the urgency to act now,” said Dr. Joseph Kanter, State Health Officer. “Over the weekend we reviewed new data from the CDC showing that while vaccination reduces one’s chance of becoming infected with COVID-19, those who do become infected with the Delta variant despite being fully vaccinated are likely at risk of transmitting it to others. This new information and other recent data showing the Delta variant is more than twice as transmissible as the original strains of COVID-19 bolster our recommendation to the Governor to put a universal mask mandate in place immediately.”
- Click hereto view the Governor’s Updated Public Health Emergency Order and Indoor Statewide Mask Mandate.
- Click hereto review data and slides presented at today’s media briefing.
As has always been the case, local leaders may implement mitigation measures that are more comprehensive and restrictive than the current state guidelines, should they feel this is best for their communities.
STATEWIDE MASK MANDATE
Face masks that properly cover the wearer’s mouth and nose should be worn indoors at all times, unless a person is in a home, under the Governor’s statewide mask mandate, which will be in place until at least September 1.
The order requires face coverings for everyone age 5 or older or enrolled in kindergarten, except for the following:
- Anyone who has a medical condition that prevents the wearing of a face covering
- Anyone who is consuming a drink or food
- Anyone who is trying to communicate with a person who is hearing impaired
- Anyone who is giving a speech for broadcast or to an audience
- Anyone temporarily removing his or her face covering for identification purposes
Face coverings are highly encouraged for those ages 2 to 4 as tolerated.
As with the Governor’s previous mandate, children younger than kindergarten age are exempted if they cannot wear a mask. However, the CDC and the Louisiana Department of Health strongly encourage indoor mask wearing in public for all children aged two and older, especially as they are not yet eligible for the COVID vaccine. Generally, LDH shares these reminders for individuals and families who are trying to stay as safe as possible during the COVID-10 pandemic:
- If you can do an activity outdoors instead of indoors, do it outdoors
- Follow good hygiene practices (wash your hands vigorously and frequently, and don’t touch your face)
- Stay away from crowded settings
- Work virtually if possible
- If you suspect you have been exposed to COVID-19, get tested immediately
- If you’re in an at-risk group, be extra careful
- Everyone who is sick or who has COVID symptoms should stay home
GUIDANCE FOR LARGE GATHERINGS
Today, the Louisiana Department of Health additionally issued guidance to the public about large event gatherings during the fourth surge of COVID-19 in Louisiana, including ways to lower risk for both vaccinated and unvaccinated people.
LDH recommends:
- Limiting the size of indoor gatherings, moving events outdoors, or hosting meetings and events virtually to reduce the likelihood of COIVD-19 spread.
- All participants of indoor meetings and events are required to be masked.
- People with underlying health conditions that make them more likely to have severe COVID complications should avoid nonessential trips outside of the home.
- Event hosts and facilities should practice strong sanitation and hygiene practices and provide hand sanitizer for those who need it.
- Spaces should be staged to accommodate at least six feet of distance between guests.
TESTING AND QUARANTINE GUIDANCE
Under guidance issued by LDH two weeks ago, all businesses should review their operations to accommodate employees in a way that reduces unnecessary contact to avoid the spread of COVID in the workplace.
In addition, all people should take a COVID test immediately after a known or suspected exposure to COVID-19 and take the following actions:
- If positive, they should isolate immediately.
- If negative, they should retest again between five and seven days post-exposure.
- If they develop symptoms of COVID-19 at any point they should test and immediately isolate pending the results.
This guidance will remain in place at least until Louisiana is safely out of its fourth COVID-19 surge, with additional guidance and mitigation measures put in place if and when necessary to slow the spread of the more contagious and virulent Delta variant and preserve hospital capacity.
At this time, the CDC advises that fully vaccinated individuals who are not experiencing COVID symptoms do not need to quarantine following an exposure to COVID-19, and LDH is not yet altering this guidance.
Anyone with symptoms of COVID-19, even those who are fully vaccinated or without a known exposure, should get tested.
Anyone who tests positive should immediately isolate. Isolation (for those who test positive for COVID-19) typically consists of:
- If symptomatic, at least 10 days since symptoms first appeared, symptoms are improving, and at least 24 hours with no fever without fever-reducing medication
- If asymptomatic but with a positive test, 10 days from the time the test sample was collected
Call 211 to find a COVID-19 testing site near you.
In Zachary, COVID-19 testing is available at FastLane urgent care for walk-ins and by appointment at Lane Family Practice and Lane Pediatrics.
HOW TO GET A COVID VACCINE IN LOUISIANA
Everyone aged 12 and older is eligible for the COVID-19 vaccine in Louisiana. The FDA has only authorized one of the three COVID-19 vaccines – from Pfizer – for children ages 12 to 17. Parents should confirm with the vaccine provider that their child is under 18 to ensure Pfizer vaccine is available before making an appointment.
- COVID-19 vaccines are widely available at 1,437 locations in all of Louisiana’s 64 parishes, including at pharmacies, hospitals, health care clinics, and doctor’s offices.
- In Zachary, vaccine appointments are available at Lane Family Practice, 654-3607.
Update – August 2, 2021
Like the majority of hospitals statewide, Lane Regional Medical Center is experiencing high volumes of COVID-19 patients and is extremely busy.
Effective today and for the next several weeks, Lane is pausing all non-urgent surgical procedures that require an overnight stay in order to keep more inpatient beds available.
Outpatient procedures that do not require an overnight stay in the hospital will continue to be scheduled and performed.
Please do not delay care when needed. Please call your doctor for medication refills, annual appointments, or if you have minor symptoms or conditions that need to be treated.
Emergency room visits may be warranted for a number of reasons, such as high fevers, difficulty breathing, cuts that require stitches, heart attack or stroke symptoms, or other life-threatening emergencies.
COVID-19 testing is available at FastLane urgent care for walk-ins and by appointment at Lane Family Practice and Lane Pediatrics. COVID-19 vaccination appointments are also available at Lane Family Practice.
Visitor Policy - Updated July 21, 2021
As we respond to a new surge of COVID-19, patient and team member safety remain our highest priority.
To ensure the safety of our hospital and community while remaining empathetic to the needs of our patients and families, we will revert back to a single entrance for patients and visitors through the Emergency Department.
- Each non-COVID-19 patient will be allowed a maximum of 1 visitor a day who is allowed to spend the night with the patient if desired. No rotating of visitors will be allowed.
- One visitor is allowed to visit patients being treated for COVID-19 during regular visiting hours - No overnight stays and no rotating of visitors will be allowed
VISITING HOURS
Visiting Hours: 8 a.m. - 6 p.m. Patient Rooms
8 a.m. - 6 p.m. Labor & Delivery / Recovery & Postpartum
SCREENING
All visitors will continue to be screened daily for symptoms, including:
- History of positive COVID-19 diagnosis within the last 10 days
- Exposure to a positive COVID-19 person within the last 14 days
- Fever greater than or equal to 100°F
- Loss of smell/taste
Screeners will be logging and screening visitors entering the facility.
If a visitor says “YES” to any of the screening symptoms or have fever at screening area, they will not be allowed entry into the facility
SAFETY
With the well-being and protection of our team, patients, and community in mind, we will require all employees, visitors, and patients to adhere to the below safety measures:
- Wear a mask
- Practice social distancing
- Practice consistent hand hygiene
- Visitors must wear a mask when caregivers enter room or when entering or leaving the building
PATIENT VISITATION
Visitors will not be allowed to rotate throughout the day during visitation hours. One visitor may stay overnight with non-Covid-19 patients.
- Inpatient Units: One visitor will be allowed per patient during designated visiting hours.
- Critical Care Units: One visitor will be allowed per patient during designated visiting hours.
- Labor & Delivery: Two visitors are allowed per patient during designated visiting hours.
- Children Visitors: No children under age 18 unless here for a procedure or end of life visitation.
- Persons Under Investigation (PUI) or confirmed COVID-19 patients:
- One visitor during regular visiting hours, except for end of life
- The visitor must wear the recommended personal protective equipment (PPE) for the duration of the visit, including a mask and remain in the room at all times.
- Emergency Department: One visitor per day. Visitor is allowed to stay all day, not restricted to visitation hours. Visitor is not allowed to swap out. Must be over 18 years of age.
- Surgery and Procedures: Patients undergoing surgery or being admitted to the hospital may have 1 designated visitor pre-procedure, and if admitted, visitors must follow the visitation guidelines.
- Outpatient Services/Appointments: Patients may have 1 visitor to accompany them during their service/appointment, not limited to visitation hours.
- Vendors/Referrals: Will be allowed for direct patient care activities.
- Gift shop or Cafeteria: Closed to the general public.
- Retail pharmacy: No customers allowed. Please call 658-6770 to fill a prescription, and a representative will deliver it to you at the ER entrance. Hours 8am-4pm
- Billing: No customers allowed. Please call 844-620-8131 for assistance. To make a payment in person, call 658-4343 and a representative will meet you at the ER entrance.
- Medical Records: No customers allowed. Please call 658-4311 for assistance.
Exceptions to the Visitor Policy outside of Regular Visiting Hours:
-
End of Life*
: A maximum of 2 visitors per patient, rotating if necessary. Remaining family waiting to see patient will be asked to wait outside or in their vehicle. Clergy will be allowed for end of life situations.
*End of life is defined as anticipated death with an active do-not-resuscitate (DNR) order in place and/or planned withdrawal of life-sustaining interventions (e.g., ventilator).
Update May 19, 2021 - COVID Vaccines
COVID-19 Vaccines for Children and Teens
Although fewer children have been infected with COVID-19 compared to adults, children can:
- Be infected with the virus that causes COVID-19
- Get sick from COVID-19
- Spread COVID-19 to others.
CDC recommends everyone 12 years and older should get a COVID-19 vaccination to help protect against COVID-19. Widespread vaccination is a critical tool to help stop the pandemic. Getting your child or teen vaccinated can bring you one step closer to enjoying the activities you miss. Children 12 years and older are able to get the Pfizer-BioNTech COVID-19 Vaccine.
Interim Public Health Recommendations for Fully Vaccinated People
- Fully vaccinated people no longer need to wear a mask or physically distance in any setting, except where required by federal, state, local, tribal, or territorial laws, rules, and regulations, including local business and workplace guidance
- Fully vaccinated people can refrain from testing following a known exposure unless they are residents or employees of a correctional or detention facility or a homeless shelter
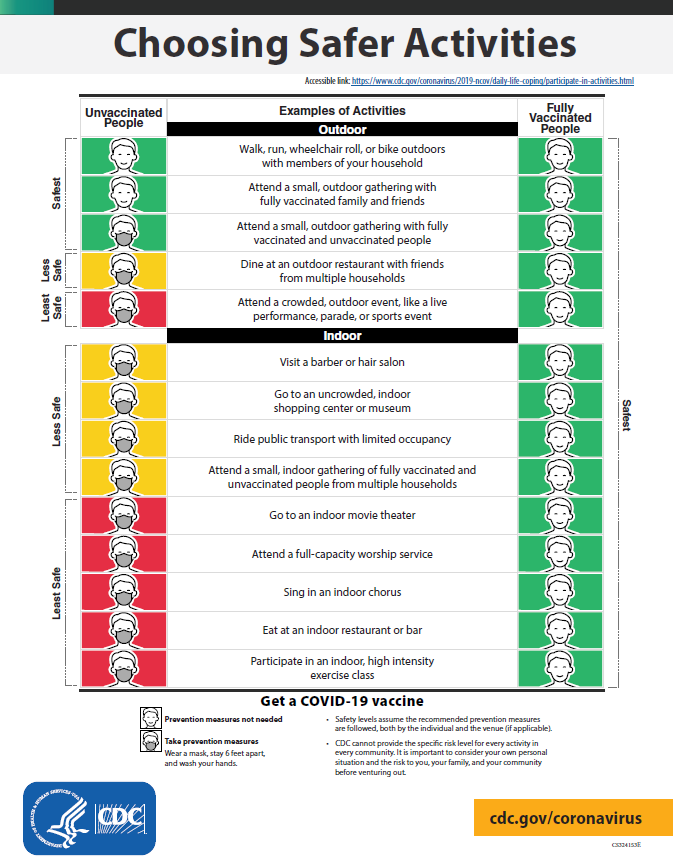
INFOGRAPHIC
If you are fully vaccinated you can start doing many things that you had stopped doing because of the pandemic.
Key Points
The following recommendations apply to non-healthcare settings. For related information for healthcare settings, visit Updated Healthcare Infection Prevention and Control Recommendations in Response to COVID-19 Vaccination.
Fully vaccinated people can:
- Resume activities without wearing masks or physically distancing, except where required by federal, state, local, tribal, or territorial laws, rules and regulations, including local business and workplace guidance
- Resume domestic travel and refrain from testing before or after travel or self-quarantine after travel
- Refrain from testing before leaving the United States for international travel (unless required by the destination) and refrain from self-quarantine after arriving back in the United States
- Refrain from testing following a known exposure, if asymptomatic, with some exceptions for specific settings
- Refrain from quarantine following a known exposure if asymptomatic
- Refrain from routine screening testing if feasible
For now, fully vaccinated people should continue to:
- Get tested if experiencing COVID-19 symptoms
- Follow CDC and health department travel requirements and recommendations
Update January 15, 2021 - Revised Visitor Guidance
As we continue to respond to COVID-19, patient and team member safety remains our highest priority to ensure the safety of our hospital and community while remaining empathetic to the needs of our patients and families.
While still limiting the number of visitors allowed, we are increasing the number of visitors allowed for non-COVID patients and will continue with the single entrance for visitors through the Emergency Department.
- Each patient will be allowed a maximum of 2 visitors a day, and one is allowed to spend the night with the patient if desired. Visitors will not be allowed to rotate throughout visiting hours.
- Visiting Hours will be remain the same:
- 8 a.m.- 8p.m. patient room visiting hours
- 8 a.m.-8 p.m. Labor& delivery/Recovery & Postpartum
- No visitors are allowed to visit patients being treated for COVID-19 except under approved circumstances -*Approved by director, house supervisor, or administration
SCREENING
Screeners will be logging and screening visitors entering the facility. All visitors will continue to be screened daily for symptoms, including:
- History of positive COVID diagnosis within the last 10 days
- Exposure to a positive COVID person within the last 14 days
- Fever greater than or equal to 100°F
- Loss of smell/taste
If a visitor says “YES” to any of the screening symptoms or has a fever at screening area, they will not be allowed entry into the facility.
SAFETY
With the well-being and protection of our team, patients, and community in mind, we will require all employees, visitors, and patients to adhere to the below safety measures:
- Wear a mask
- Practice social distancing
- Practice consistent hand hygiene
- Visitors must wear a mask when caregivers enter room and when entering or leaving the building
Patient Visitation:
- Inpatient Units- Two visitors will be allowed during normal visiting hours.
- Critical Care Units- Two visitors will be allowed during normal visiting hours.
- Labor & Delivery- Four visitors are allowed per patient during normal visiting hours.
Visitors will not be allowed to rotate throughout the day during visitation hours.
One visitor may stay with the patient overnight
- Children Visitors- No children under age 18 allowed, unless here for a procedure or end of life visitation.
- Persons Under Investigation (PUI) or confirmed COVID-19 patients:
- No visitors, except for end of
- If a visitor is allowed under the outlined exceptions, the visitor must wear the recommended personal protective equipment (PPE) for the duration of the visit, including a mask.
- Vendors/Referrals- Will be allowed for direct patient care activities.
- For the viewing of decedent bodies- If a visitor needs to view a decedent body, security will escort the visitor to the room for viewing and kindly escort them back to the facility entrance for departure.
- Retail Pharmacy/Billing/Medical Records- Customers are allowed, without visitors.
- Gift Shop or Cafeteria - No customers will allowed to enter the hospital for the sole purpose of going to these areas.
Exceptions to the Visitor Policy outside of the visiting hours:
- End of Life- A maximum of 4 visitors per room, rotating if necessary. Remaining family waiting to see the patient will be asked to wait outside or in their vehicle. The hospital will limit the number to 8 visitors per patient unless approved by director, house supervisor or administration.
- End of life refers to a final period in a person’s life, in which it is medically obvious that death is imminent or a terminal moribund state cannot be prevented.
- Surgery and Procedures- Patients undergoing surgery or being admitted to the hospital may have designated visitors pre-procedure, and if admitted, the visitors must follow the visitation guidelines.
- Outpatient services/Appointments-Patients may have 1 visitor to accompany them during their service/appointment not limited to visitation hours. Emergency Department- One visitor (over 18 year of age) is allowed during the emergency department stay, all day, not restricted to visitation hours.
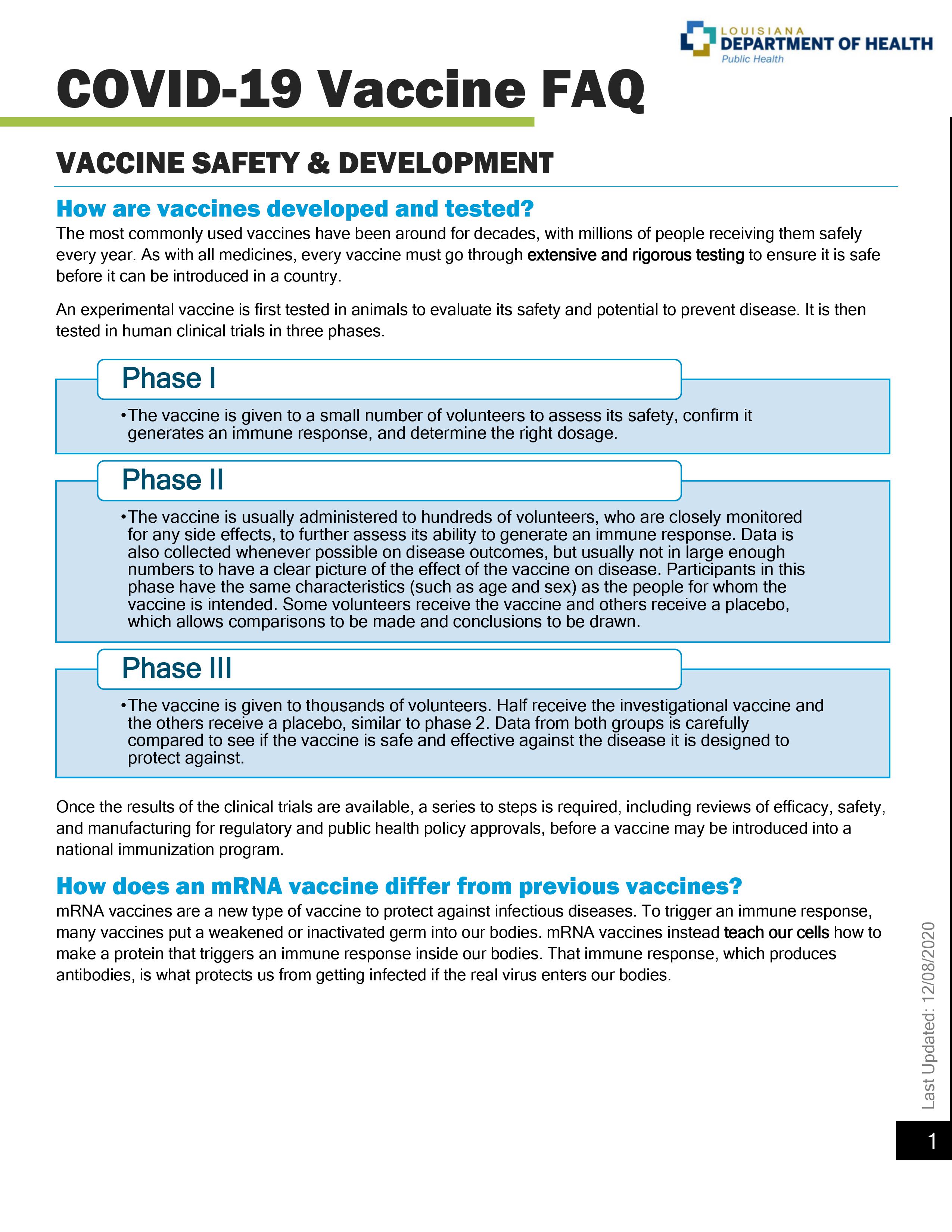
Update December 11, 2020 - COVID-19 Vaccine FAQ
Update November 24, 2020 - Personal and Social Activities
What you need to know
- Stay home if sick.
- Wear masks in public settings, like on public and mass transportation, at events and gatherings, and anywhere they will be around other people.
- Use social distancing (stay at least 6 feet away from others).
- Before you go, call and ask what extra prevention strategies they are using, like requiring staff to wear masks.
- Wash your hands with soap and water for at least 20 seconds when you get home.
Gatherings or Cook-Outs
Remind guests to stay home if they are sick

- Remind invited guests to stay home if they have been exposed to COVID-19 in the last 14 days or are showing COVID-19 symptoms. Anyone who has had close contact with a person who has COVID-19 should also stay home and monitor their health. Invited guests who live with those at higher risk should also consider the potential risk to their loved ones.
- Consider keeping a list of guests who attended for potential future contact tracing needs.
Encourage social distancing
- Host your gathering outdoors, when possible. If this is not feasible, make sure the room or space is well-ventilated (for example, open a window).
- Arrange tables and chairs to allow for social distancing. People from the same household can be in groups together and don’t need to be 6 feet apart – just 6 feet away from other families.
- If planning activities for adults and/or kids, consider those where social distancing can be maintained, like sidewalk chalk art or frisbee.
- When guests arrive, minimize gestures that promote close contact. For example, don’t shake hands, do elbow bumps, or give hugs. Instead wave and verbally greet them.
Wear masks
- Wear masks when less than 6 feet apart from people or indoors.
- Consider providing masks for guests or asking them to bring their own.
Clean hands often
- Consider providing hand sanitizer in addition to clearly marked hand washing areas.
- Wash your hands for at least 20 seconds when entering and exiting social gatherings. If soap and water are not readily available, use a hand sanitizer that contains at least 60% alcohol. Cover all surfaces of your hands and rub them together until they feel dry.
- Make sure there is adequate soap or hand sanitizer containing at least 60% alcohol available in the restrooms and encourage guests not to form a line at the door. Consider also providing cleaning supplies that allow guests to wipe down surfaces before they leave.
- Remind guests to wash their hands before serving or eating food.
- Use single-use hand towels or paper towels for drying hands so guests do not share a towel.
Limit the number of people handling or serving food
- Encourage guests to bring their own food and drinks.
- Limit people going in and out of the areas where food is being prepared or handled, such as in the kitchen or around the grill, if possible.
- If serving any food, consider identifying one person to serve all food so that multiple people are not handling the serving utensils.
- Use single-use options or identify one person to serve sharable items, like salad dressings, food containers, and condiments, so that multiple people are not handling the items.
Limit contact with commonly touched surfaces or shared items
- Use touchless garbage cans or pails.
- Use gloves when removing garbage bags or handling and disposing of trash. Wash hands after removing gloves.
- Clean and disinfect commonly touched surfaces and any shared items between users when feasible.
- If you choose to use any shared items that are reusable (e.g., seating covers, tablecloths, linen napkins), wash, clean, and sanitize them after the event.
Attending an Event or Gathering
Prepare before you go:
- Stay home if you have been diagnosed with COVID-19 (symptoms of COVID-19) , if you are waiting for COVID-19 test results, or may have been exposed to someone with COVID-19.
- Check with the organizer or event venue for updated information about any COVID-19 safety guidelines and if they have steps in place to prevent the spread of the virus.
- Prioritize attending outdoor activities over indoor activities and stay within your local area as much as possible.
- Bring supplies to help you and others stay healthy—for example, masks (bring extra), hand sanitizer with at least 60% alcohol, and drinking water.
Use social distancing and limit physical contact
- Maintain a distance of at least 6 feet or more from people who don’t live in your household. Be particularly mindful in areas where it may harder to keep this distance, such as check-in areas, parking lots, and routes of entry and exit.
- Select seating or determine where to stand based on the ability to keep 6 feet of space from people who don’t live in your household, including if you will be eating or drinking.
- Arrive to the event early or at off-peak times to avoid crowding and congested areas.
- Avoid using restroom facilities or concession areas at high traffic times, such as intermission, half-time, or immediately at the end of the event.
Wear masks
- Wear a mask when interacting with other people to minimize the risk of transmitting the virus.
- Wearing masks is most important when social distancing is difficult.
- Masks are strongly encouraged in settings where individuals might raise their voices, such as shouting, chanting, or singing.
Limit contact with commonly touched surfaces or shared items
- Use touchless garbage cans or pails and cashless payment options when possible. Otherwise, exchange cash or card by placing payment in a receipt tray, if available, or on the counter.
- Avoid any self-serve food or drink options, such as buffets, salad bars, and condiment or drink stations. Use grab-and-go meal options, if available.
- Use disposable food service items including utensils and dishes, if available.
- Wash your hands with soap and water for at least 20 seconds or use hand sanitizer immediately before eating food or after touching any common surfaces like hand railings, payment kiosks, door handles, and toilets.
Dining at a Restaurant
Check the restaurant’s COVID-19 prevention practices before you go

- Check the restaurant’s website and social media to see if they have updated their information to address any COVID-19 safety guidelines.
- Before you go to the restaurant, call and ask if all staff are wearing masks while at work.
- Ask about options for self-parking to remove the need for a valet service.
Wear masks when less than 6 feet apart from other people or indoors
Take steps to protect yourself at the restaurant
- Wear masks when less than 6 feet apart from other people or indoors.
- Take precautions – like wearing a mask as much as possible when not eating and maintaining a proper social distance if you are dining with others who don’t live with you.
- Maintain a social distance of 6 feet or more in any entryway, hallway, or waiting area.
- When possible, sit outside at tables spaced at least 6 feet apart from other people.
- When possible, choose food and drink options that are not self-serve to limit the use of shared serving utensils, handles, buttons, or touchscreens.
Clean hands
- Wash your hands for at least 20 seconds when entering and exiting the restaurant. If soap and water are not readily available, use a hand sanitizer that contains at least 60% alcohol. Cover all surfaces of your hands and rub them together until they feel dry.
Before using the restroom, make sure there is enough soap and a way to dry your hands (e.g., paper towels, hand dryer), or hand sanitizer containing at least 60% alcohol
Using Gyms or Fitness Centers
Prepare before you go
- Use options for online reservations and check-in systems when available.
- Look for any extra prevention practices being implemented by the facility, such as new plexiglass barriers, staff wearing masks, and closing of shared locker room space.
- Be prepared that locker room access may be limited to the restroom area only, prohibiting the use of shower and changing areas.
Limit activity indoors, especially group activities
- Seek facilities with outdoor space or options for virtual classes and training sessions as much as possible.
- Limit attendance at indoor group training sessions. If you do attend such a session, maintain as much distance as possible between yourself and other individuals, and use masks if they do not interfere with your activity. If you need to be indoors, open windows to increase airflow throughout the space.
Use social distancing and limit physical contact
- Maintain at least 6 feet of separation as much as possible in areas that may lead to close contact (within 6 feet) among other people, such as weight rooms, group fitness studios, pools and saunas, courts and fields, walking/running tracks, locker rooms, check-in areas, parking lots, and routes of entry and exit.
- Don’t shake hands, give high-fives, do elbow bumps, or touch others because close contact increases the risk of acquiring COVID-19.
Take extra precautions with shared equipment
- Ensure equipment is clean and disinfected. Wipe down machines and equipment with disinfecting wipes and use hand sanitizer that contains at least 60% alcohol before using machines.
- Do not share items that cannot be cleaned, sanitized, or disinfected between use, such as resistance bands and weightlifting belts.
Wear a mask
- Wear a mask when interacting with other people to minimize the risk of transmitting the virus.
- Wearing masks is most important when physical distancing is difficult and when exercise type and intensity allows. Consider doing any vigorous-intensity exercise outside when possible and stay at least 6 feet away from other participants, trainers, and clients if unable to wear a mask.
- If possible, wear a mask when walking on an indoor track or when doing stretching or low-intensity forms of yoga indoors.
- Wash your hands before adjusting your mask—review information about proper use, removal, and washing of masks.
Going to a Nail Salon

Wear a mask
Prepare for your appointment
- Book services in advance to remove the need for waiting in a lobby with other people. If you must wait, maintain social distance.
- Before you go, call and ask if all staff are wearing masks at work and if there are physical barriers to minimize risk of transmission (e.g., plexiglass barriers).
- If offered by the salon, wait in your car or outside until you can be contacted by mobile phone when it is your turn to be seen for an appointment.
Wear a mask
- Wear a mask at all times when inside the salon.
Wash hands often and limit contact with common surfaces or items
- Wash your hands or use hand sanitizer immediately before receiving your service and after touching any common surfaces like curing lamps, countertops, doorknobs, toilets, tables, light switches, phones, faucets, sinks, and keyboards.
- Use cashless payment options when possible. If not available, ensure that cash and cards are handled with care by employees either by changing gloves between each transaction or with use of hand sanitizer between clients.
- Look for no-touch waste baskets at the cash registers and in the restrooms.
Visiting a Library

Choose digital materials or use curbside pick-up, when possible
Use curbside pickup or choose digital materials
- Use online reservation and advance-order checkout systems, if possible.
- Choose digital over print materials, if possible.
- Request a curbside pick-up if available and use masks during pick-up exchanges.
Clean hands when handling shared items or electronics
- Wash your hands before and after exchanges.
- Clean and disinfect electronics (laptops) and library materials in plastic containers (CDs, audio books) during returns and/or exchanges.
- If allowed and available inside the library, use computer stations one person at a time. Ensure they are cleaned before use and use a disinfectant wipe on the mouse and keyboard.
Traveling Overnight

Wear a mask in the lobby or other common areas
Check the hotel’s COVID-19 prevention practices before you go
- Use options for online reservation and check-in, mobile room key, and contactless payment.
- Before you go, call and ask if all staff are wearing masks at work.
- Look for any extra prevention practices being implemented by the hotel, such as plexiglass barriers at check-in counters, and physical distancing signs in the lobby.
- Ask if the hotel has updated policies about cleaning and disinfecting or removing frequently touched surfaces and items (such as pens, room keys, tables, phones, doorknobs, light switches, elevator buttons, water fountains, ATMs/card payment stations, business center computers and printers, ice/vending machines, and remote controls).
Wear masks and limit close contact with others
- Wear a mask in the lobby or other common areas.
- Minimize use of areas that may lead to close contact (within 6 feet) with other people as much as possible, like break rooms, outside patios, inside lounging areas, dining areas/kitchens, game rooms, pools, hot tubs, saunas, spas, salons, and fitness centers.
- Consider taking the stairs. Otherwise wait to use the elevator until you can either ride alone or only with people from your household.
Choose contactless options, when possible
- Request contactless delivery for any room service order.
- If you are considering cleaning your travel lodgings, see CDC’s guidance on how to clean and disinfect.
Protect yourself and others when you travel away your community
- Learn more about safely planning travel during the COVID-19 outbreak.
Update November 20, 2020 – Considerations for Wearing a Mask to Help Slow the Spread of COVID-19
Considerations for Wearing Masks
To Help Slow the Spread of COVID-19
What you need to know
- People age 2 and older should wear masks in public settings and when around people who don’t live in their household.
- Masks offer some protection to you and are also meant to protect those around you, in case you are unknowingly infected with the virus that causes COVID-19.
- A mask is NOT a substitute for social distancing. Masks should still be worn in addition to staying at least 6 feet apart.
- Wash your hands with soap and water for at least 20 seconds or use hand sanitizer with at least 60% alcohol after touching or removing your mask.
- Masks may not be necessary when you are outside by yourself away from others, or with other people who live in your household. However, some localities may have mask mandates while out in public and these mandates should always be followed.
- CDC is still studying the effectiveness of different types of masks and will update our recommendations as new scientific evidence becomes available.
Evidence for Effectiveness of Masks

Your mask helps protect those around you
COVID-19 spreads mainly from person to person through respiratory droplets. Respiratory droplets travel into the air when you cough, sneeze, talk, shout, or sing. These droplets can then land in the mouths or noses of people who are near you or they may breathe these droplets in.
Masks are a simple barrier to help prevent your respiratory droplets from reaching others. Studies show that masks reduce the spray of droplets when worn over the nose and mouth.
You should wear a mask, even if you do not feel sick. This is because several studies have found that people with COVID-19 who never develop symptoms (asymptomatic) and those who are not yet showing symptoms (pre-symptomatic) can still spread the virus to other people. The main function of wearing a mask is to protect those around you, in case you are infected but not showing symptoms.
It is especially important to wear a mask when you are unable to stay at least 6 feet apart from others since COVID-19 spreads mainly among people who are in close contact with one another (within about 6 feet).
Your mask offers some protection to you
A cloth mask also offers some protection to you too. How well it protects you from breathing in the virus likely depends on the fabrics used and how your mask is made (e.g. the type of fabric, the number of layers of fabric, how well the mask fits). CDC is currently studying these factors.
Who Should or Should Not Wear a Mask
Who should wear a mask
Everyone 2 years of age and older should wear a mask in public settings and when they are around people who do not live in their household.
Wear a mask when caring for someone who is sick with COVID-19 (whether at home or in a non-healthcare setting). If you are sick with COVID-19 or think you may have COVID-19, wear a mask when you need to be around other people or animals, even in your own home.
CDC recognizes there are specific instances when wearing a mask may not be feasible. In these instances, consider adaptations and alternatives.
Who should not wear a mask
Masks should not be worn by
- Children younger than 2 years old
- Anyone who has trouble breathing
- Anyone who is unconscious, incapacitated or otherwise unable to remove the mask without assistance
- Wearing masks may be difficult for some people with sensory, cognitive, or behavioral issues. If they are unable to wear a mask properly or cannot tolerate a mask, they should not wear one, and adaptations and alternatives should be considered
Types of masks
Some masks work better to help stop the spread of COVID-19 outside of healthcare settings. Medical masks and N-95 respirators should not be used because they should be conserved for healthcare workers.
Recommended
Not Recommended

Non-medical disposable masks

Masks that fit properly (snugly around the nose and chin with no large gaps around the sides of the face)

Masks that do not fit properly (large gaps, too loose or too tight)

Masks made with breathable fabric (such as cotton)

Masks made from materials that are hard to breathe through (such as plastic or leather)

Masks made with tightly woven fabric (i.e., fabrics that do not let light pass through when held up to a light source)

Masks made from loosely woven fabric or that are knitted, i.e., fabrics that let light pass through

Masks with two or three layers

Masks with one layer

Masks with inner filter pockets

Masks with exhalation valves or vents
Cloth masks
The most effective fabrics for cloth masks are
- Tightly woven fabrics, such as cotton and cotton blends
- Breathable
- Two or three layers
Less effective fabrics for cloth masks are
- Loosely woven fabrics, such as loose knit fabrics
- Difficult to breathe through (like plastic or leather)
- Single layer
CDC is currently studying the effectiveness of various cloth mask materials. We will update this guidance as we learn more.
Non-medical disposable masks
Disposable face masks are single-use masks. They are sold online and through large retail stores. These are not the same as surgical or other medical masks.
You may prefer using disposable masks in situations where your mask is likely to get wet or dirty. As with cloth masks, make sure your disposable mask fits close to your face without large side-gaps and completely covers your nose and mouth. Bring extra disposable masks with you in case you need to change out a dirty or wet mask.

Masks with exhalation valves or vents
CDC does not recommend using masks with exhalation valves or vents because this type of mask may not prevent you from spreading COVID-19 to others. The hole in the material may allow your respiratory droplets to escape and reach others. Research on the effectiveness of these types of masks is ongoing.

Surgical masks and respirators
Do not use surgical masks and respirators that are meant for healthcare workers. Currently, surgical masks and respirators are critical supplies that should be reserved for healthcare workers and other medical first responders to prevent supply shortages.

Clear masks or cloth masks with a clear plastic panel
Clear masks or cloth masks with a clear plastic panel are an alternative type of mask for people who interact with
- People who are deaf or hard of hearing
- Young children or students learning to read
- Students learning a new language
- People with disabilities
- People who need to see the proper shape of the mouth for making appropriate vowel sounds, e.g., in singing

If you use this type of mask, make sure
- You can breathe easily
- Excess moisture does not collect on the inside of the mask
- You remove the mask before sleeping, since the plastic part could form a seal around your mouth and nose and make it hard to breathe
The FDA recently cleared a transparent pdf iconexternal iconmedical mask. These transparent medical masks should be reserved for use by healthcare workers and patients who require them.
Other Types of Face Protection
CDC does not recommend using face shields or goggles as a substitute for masks. Do NOT put a plastic face shield (or a mask) on newborns or infants.
Face shields and goggles are primarily used to protect the eyes of the person wearing it. Goggles do not cover the nose and mouth. Face shields have large gaps below and alongside the face, where your respiratory droplets may escape and reach others around you. At this time, we do not know how much protection a face shield provides to people around you. However, wearing a mask may not be feasible in every situation for some people.

Face sheilds and goggles
For example, people who interact with those who are deaf or hearing impaired may find that a face shield is better than a mask when communicating. If you must wear a face shield instead of a mask:
- Choose a face shield that wraps around the sides of your face and extends below your chin or a hooded face shield. This is based on the limited available data that suggest these types of face shields are better at preventing spray of respiratory droplets.
- Wash your hands before and after removing the face shield. Avoid touching your eyes, nose, and mouth when removing it.
- Clean and disinfect reusable face shields according to the manufacturer’s instructions or by following CDC face shield cleaning instructions. If you use a disposable face shield, wear it once and throw it away according to the manufacturer’s instructions.
Mask Adaptations and Alternatives
CDC recognizes that wearing masks may not be possible in every situation or for some people. Those who cannot wear a mask are urged to prioritize virtual engagement when possible. For in-person activities, we have provided a few examples of what you can do to make wearing a mask more feasible and how to reduce the spread of COVID-19 if you cannot wear a mask.
Situations where wearing a mask may not be possible
- Make sure to maintain physical distance from others when you cannot wear a mask.
Dining
- CDC recommends wearing a mask while dining in a restaurant except when actively eating or drinking.
Water activities
- Do not wear a mask when doing activities that may get your mask wet, like swimming at the beach or pool. A wet mask can make it difficult to breathe and may not work as well when wet.
High intensity activities
- Masks should be used in public settings, but if you are unable to wear a mask because of difficulty breathing during high intensity activities, choose a location with greater ventilation and air exchange (for instance, outdoors versus indoors) and where you can keep at least 6 feet from others during the activity.
- If you are able to wear a mask, remove your mask if it gets moist from sweat and replace it with a clean mask.
- Opt for an activity that does not require using mouth guards or helmets. Wearing a mask with these types of protective equipment is not safe if it makes it hard to breathe.
- Supervise children who are wearing a mask while playing sports.
Certain groups of people who may find it difficult to wear a mask
Some children 2 years and older, and people of any age with certain disabilities
Appropriate and consistent use of masks may be challenging for some children and for people of any age with certain disabilities, including cognitive, intellectual, developmental, sensory, and behavioral disorders.
When deciding if children and people with certain disabilities should wear a mask, determine if they can:
- Use a mask correctly
- Avoid frequent touching of the mask and their face
- Limit sucking, drooling, or having excess saliva on the mask
- Remove the mask without assistance
If children and people with certain disabilities are unable to wear a mask properly or cannot tolerate a mask, they should not wear one.
Those caring for children and people with certain disabilities who may not be able to wear a mask should
- Ask their healthcare provider for advice about their wearing a mask
- Ensure proper mask size and fit
- Remove their mask before sleeping, napping, when they may fall asleep (such as in a car seat or stroller), and in situations when continual supervision is not possible
- Consider prioritizing wearing a mask when it is difficult to keep at least 6 feet from others (for example, during carpool drop off or pick up, or when standing in line at schools or stores)
Masks should not be worn by:
- Children younger than 2 years old
- Anyone who has trouble breathing
- Anyone who is unconscious, incapacitated, or otherwise unable to remove the mask without assistance
People who are deaf or hard of hearing, and those who will interact with people who are hearing impaired
If you interact with people who rely on reading lips, you may have difficulty communicating while wearing a mask.
- Consider wearing a clear mask or a cloth mask with a clear panel
- If you are not able to get a clear mask, consider using written communication, closed captioning, or decreasing background noise to make communication possible while wearing a mask that blocks lips
People with certain underlying medical conditions
Most people with underlying medical conditions can and should wear masks.
- If you have respiratory conditions and are concerned about wearing a mask safely, discuss with your healthcare provider the benefits and potential risks of wearing a mask.
- If you have asthma, you can wear a mask. Discuss with your healthcare provider if you have any concerns about wearing a mask.
Outdoor workers
If you work in a setting where masks could increase the risk of heat-related illness or cause safety concerns (for example, straps getting caught in machinery):
- Discuss with an occupational safety and health professional about what mask would be suitable.
- Prioritize wearing masks when in close contact with other people, like during group travel or shift meetings, and remove masks when social distancing is maintained. Some localities may require wearing masks in public outdoors, and these requirements should be followed.
Mask use and carbon dioxide
Wearing a mask does not raise the carbon dioxide (CO2) level in the air you breathe
A cloth mask does not provide an airtight fit across the face. The CO2 completely escapes into the air through and around the sides of the cloth mask when you breathe out or talk. CO2 is small enough to easily pass through any cloth mask material. In contrast, the virus that causes COVID-19 is much larger than CO2, so it cannot pass as easily through a properly designed and properly worn cloth mask.
Update September 21, 2020 - Phase 3, Visitor Policy
As we continue to respond to COVID-19, patient and team member safety remain our highest priority.
To ensure the safety of our hospital and community while remaining empathetic to the needs of our patients and families, we are again adjusting our visitor policies as Louisiana moves to Phase 3 of reopening.
We will continue with the single entrance for visitors through the Emergency Department while increasing the number of visitors allowed for non-COVID-19 patients:
Visitation
Patient Visitation: Visitors will be allowed to rotate throughout the day:
- Inpatient Units - Two visitors will be allowed during normal visiting hours. One is allowed to spend the night with the patient if desired, and visitors will be allowed to rotate throughout visiting hours.
- Critical Care Units - Two visitors will be allowed during normal visiting hours.
- Labor & Delivery - Four visitors are allowed per patient during normal visiting hours.
- Children Visitors: No children under age 18 unless here for a procedure or end of life visitation.
- Persons Under Investigation (PUI) or confirmed positive COVID-19 patients:
- No visitors, except for end of life*.
- If a visitor is allowed under the outlined exceptions, the visitor must wear the recommended personal protective equipment (PPE) for the duration of the visit, including a mask.
- Emergency Department: One visitor per day. Visitor is allowed to stay all day, not restricted to visitation hours. Visitor is not allowed to swap out. Must be over 18 years of age.
- Surgery and Procedures: Patients undergoing surgery or being admitted to the hospital may have 1 designated visitor pre-procedure, and if admitted, visitors must follow the visitation guidelines.
- Outpatient Services/Appointments: Patients may have 1 visitor to accompany them during their service/appointment, not limited to visitation hours.
Visiting Hours will remain the same:
- 8 a.m. – 10 p.m. Patient Rooms
- 8 a.m. - 8 p.m. Labor & Delivery/Recovery & Postpartum
Vendors/Referrals: Vendors will be allowed for direct patient care activities.
Retail Pharmacy/Billing/Medical Records: Customers are allowed.
Exceptions to the Visitor Policy Outside of Regular Visiting Hours:
- End of Life: Patients admitted for end of life evaluation and treatment, or patients being evaluated for and/or receiving hospice care, including PUIs and COVID-19 positive patients, may have two visitors and may rotate. Clergy will be allowed for end of life situations.
- *End of life is defined as anticipated death with an active do-not-resuscitate (DNR) order in place and/or planned withdrawal of life-sustaining interventions (e.g., ventilator).
Screening
All visitors will continue to be screened daily for symptoms, including:
- History of positive COVID diagnosis within the last 10 days
- Exposure to a positive COVID person within the last 10 days
- Fever greater than or equal to 4°F
- Cough
- Shortness of breath or difficulty breathing
- Sore throat
- Congestion that differs from their typical seasonal allergies
- Body aches
- Fatigue
- Loss of smell/taste
- Diarrhea
Security officers will be logging and screening visitors entering the facility. If a visitor says “YES” to any of the screening symptoms, they will not be allowed entry into the facility.
Safety
With the well-being and protection of our team, patients, and community in mind, we will require all employees, visitors, and patients to adhere to the following safety measures:
- Wear a mask
- Practice social distancing
- Practice consistent hand hygiene
- Visitors must wear a mask when caregivers enter room or when entering or leaving the building
------------------------------------------------------------------------------------------------------------------------------------------------------
Update August 18, 2020 - COVID-19 Testing
Prior to using our services for treatment of COVID-19 symptoms or exposure, please note:
1. You will see a provider and your insurance will be charged for the provider visit.2. Most insurance companies are covering 100% of the cost for COVID-19 treatment and testing. However, some insurance companies, including BCBS, have not covered the rapid COVID- 19 test at 100%. You are responsible for understanding how your treatment will be covered by your health plan.
- Patients exhibiting COVID-19 symptoms will receive the rapid test that provides results within 24 hours.
- Patients who have been exposed to COVID-19 but do not have symptoms will receive the standard non-rapid test that provides results with 2-3 days.
- Antibody testing is available for patients who believe they may have contracted COVID-19 in the past.
3. The cash charge and insurance charge for each test will be different. The cash price for rapid COVID testing is $210. The cash price for non-rapid COVID testing is $100. The cash price for antibody testing is $100. The insurance price will vary depending on what health plan you use. You are responsible for your health plan’s co-pays and/or deductibles for the provider visit and testing.
To schedule a COVID-19 testing visit, please call ahead for instructions:
FastLane Urgent Care Walk-in Clinic, 19900 Old Scenic Highway, 225-570-2618.
Open: Mon - Fri, 7a.m. - 8p.m.; Sat & Sun, 9am. - 6p.m.
Lane Family Practice, 2335 Church Street, 225-654-3607.
Open: Mon - Fri, 7a.m. - 5p.m.
------------------------------------------------------------------------------------------------------------------------------------------------------
Update June 8, 2020 - Phase 2
During Phase 2, Lane continues to operate with extra precautions in place to keep our patients and staff safe:
- All Hospital Services are Open - including outpatient Lab/Imaging tests, procedures, and surgeries
- The Emergency Room, hospital, and clinics have completely separate areas for testing and treating suspected COVID-19 patients. Please do not let the fear of contracting COVID-19 keep you from seeking lifesaving care.
- Masks are required, please bring your own mask from home
- Limit of one visitor per patient, per day
- All Lane Clinics are Open. Our providers are seeing patients in person or via tele-medicine. Click Here to make an appointment.
Lane Regional Medical Center is offering both COVID-19 Testing and COVID-19 Antibody Testing at Lane Family Practice and FASTLane Walk-in Clinic.
COVID-19 Antibody Testing
Please note: You will have to see a provider before being tested.
Lane Family Practice
2335 Church Street, Zachary
Call 654-3607 to schedule an appointment.
FASTLane Walk-in Clinic
19900 Old Scenic Highway, Zachary
Mon – Fri: 7 a.m. – 8 p.m.
Sat & Sun: 9 a.m. – 6 p.m.
570-2618
What is the COVID-19 Antibody Test?
The COVID-19 Antibody Test will determine the presence of antibodies to SARS-CoV-19, the virus that causes COVID-19. This test has a 98.6% accuracy rate.
Who should get a COVID-19 Antibody Test?
It is best for:
- those who have experienced COVID-19 signs and symptoms
OR - those who had a known exposure to someone who tested positive for COVID-19
When should I get the COVID-19 Antibody Test?
It is best to wait 14 days after initial symptoms or exposure before being tested for COVID-19 antibodies.
Why should I get a COVID-19 Antibody Test?
The Antibody Test is not required. You should get the Antibody Test if you want to know if you’ve had the COVID-19 virus, or not.
How is the Antibody Test performed?
A small blood sample will be drawn and sent to LabCorp for analysis.
How long will it take to get my results?
Approximately 2-3 days.
What does a negative test result mean?
A negative test result indicates you have not developed detectable antibodies. While contingent on a variety of factors, this could be due to testing too early, the absence of exposure to the virus, or a weakened immune system because of conditions or treatments that suppress immune function such as chemotherapy or HIV/AIDS.
What does a positive test result mean?
A positive test result indicates you have likely produced an immune response to the SARS-CoV-2 virus. This is not a guarantee you are immune to COVID-19. If you had an infection with another strain of coronavirus, such as the common cold, you could potentially have a positive result as well.
For additional questions, please contact your healthcare provider at Lane Family Practice or FASTLane Walk-in Clinic.
------------------------------------------------------------------------------------------------------------------------------------------------------
Visitor Update – 5-15-2020
For the safety of our patients, team members, and community:
ALL PATIENTS AND VISITORS MUST WEAR A MASK
Patients and visitors are asked to enter through the Emergency Room entrance.
Visitor limits:
- In-patients and Out-patients: 1 visitor per patient per day
- Respiratory isolation patients – no visitors allowed at this time
- ER: 1 visitor per patient
- Labor & Delivery: 1 visitor per patient per day
- Nursing Home: no visitors allowed at this time
- No children under the age of 12 allowed to visit at this time
- Exceptions may be made if the patient’s healthcare team believes visitation is essential
Other:
- Retail pharmacy – call 658-6770 to refill or pick up prescriptions
- Billing – for questions or to make a payment by phone, call 844-620-8131. For clinic or cash payments, call 658-4343, 8:30 am – 4 pm
- Medical Records – call 658-4311 and leave a message with call back number, name of patient, date of birth, and date of service if known.
_______________________________________________________________________________
Safety Precautions in Place for Lane Clinics and Emergency Rooms
There is nothing more important than your health. Please know we are following state guidelines and taking every precaution when you come into a Lane clinic or Lane emergency room.
CLINICS
At all Lane clinics, we are committed to providing you safe, convenient and effective care. We encourage you to seek the healthcare services you may have been postponing.
Here a few EXTRA precautions we have in place for your safety, and the safety of those around you:
- Masks – Everyone is required to wear a mask when entering the clinic at this time, including patients, staff members, and providers. Please bring your mask with you when you come.
- Screening – All patients will be screened for COVID-19 symptoms by phone prior to their appointment and again upon arrival. Staff members continue to be screened before work each day, wash their hands before and after every patient interaction, and wear Personal Protective Equipment (PPE).
- Disinfecting – We continue to disinfect the clinic throughout the day, especially in between patients. A deep cleaning of the entire clinic is done every evening.
- Social Distancing – Patients have the choice to wait inside the waiting room or in their vehicle. Waiting rooms are arranged to maximize social distancing with designated sick and well seating sections. Only well patients are allowed in common waiting areas for lab and x-ray. Sick patients will have labs drawn in their exam room, and/or will wait in their exam room until it’s time to be escorted to and from imaging for x-rays.
- Visitors – Patients are allowed to bring one visitor.
- Appointments – All clinics are seeing patients in person. Tele-medicine appointments are also available from the comfort of your home.
CALL TO SCHEDULE YOUR IN-PERSON OR TELE-MEDICINE APPOINTMENT TODAY.
Lane Family Practice – 654-3607
FASTLane Urgent Care – 570-2618
Lane OB/GYN – 658-1303
Lane Pediatrics – 658-4070
Lane Gastroenterology – 658-6780
Lane Surgery Group – 570-2489
Lane Audiology – 658-4154
Lane Cancer Center – 658-4400
Lane Wound Care & Hyperbarics – 658-4110
Lane Cardiovascular Center – 654-1559
Lane Outpatient Therapy – 658-4578
EMERGENCY ROOM
The Lane Regional Medical Center Emergency Room is safe and clean. Please don’t delay life-saving care in the ER because of COVID-19 fears. Ignoring signs and symptoms of stroke or heart attack puts you at an even greater risk.
EXTRA safety precautions are in place to maximize your safety in the ER:
- We have completely separate areas for testing and treating suspected coronavirus patients.
- As we do throughout the hospital, staff members are assigned to only one area - either regular patients or suspected COVID-19 patients - as to not spread possible infection between patients.
- Everyone is required to wear a mask when entering the hospital, including patients, staff and physicians. Please bring your mask with you when you come.
- All patients and staff are screened for COVID symptoms and temperatures taken upon arrival.
- We continue to thoroughly disinfect the unit throughout the day, with deep cleanings in between patients.
- If needed, there are two separate waiting rooms, one for suspected COVID-19 patients and another for non-COVID related illnesses and injuries.
- Patients are allowed to bring one visitor.
Thank you for trusting us with your care. Our mission is to provide exceptional healthcare services to every patient, every time.
----------------------------------------------------------------------------------------------------------------------------------------------
CDC Adds 6 Symptoms
The Centers for Disease Control and Prevention added six more symptoms of the novel coronavirus to its list, suggesting health experts are learning more about the growing number of ways physicians see the virus affecting patients.
Previously, the CDC listed just three known symptoms: shortness of breath, cough and fever.
The six additional symptoms are:
- Chills
- Repeated shaking with chills
- Muscle pain
- Headache
- Sore throat
- New loss of taste or smell
The symptoms usually appear within two to 14 days after exposure to the virus.
-----------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------
Avoid Coronavirus Scams
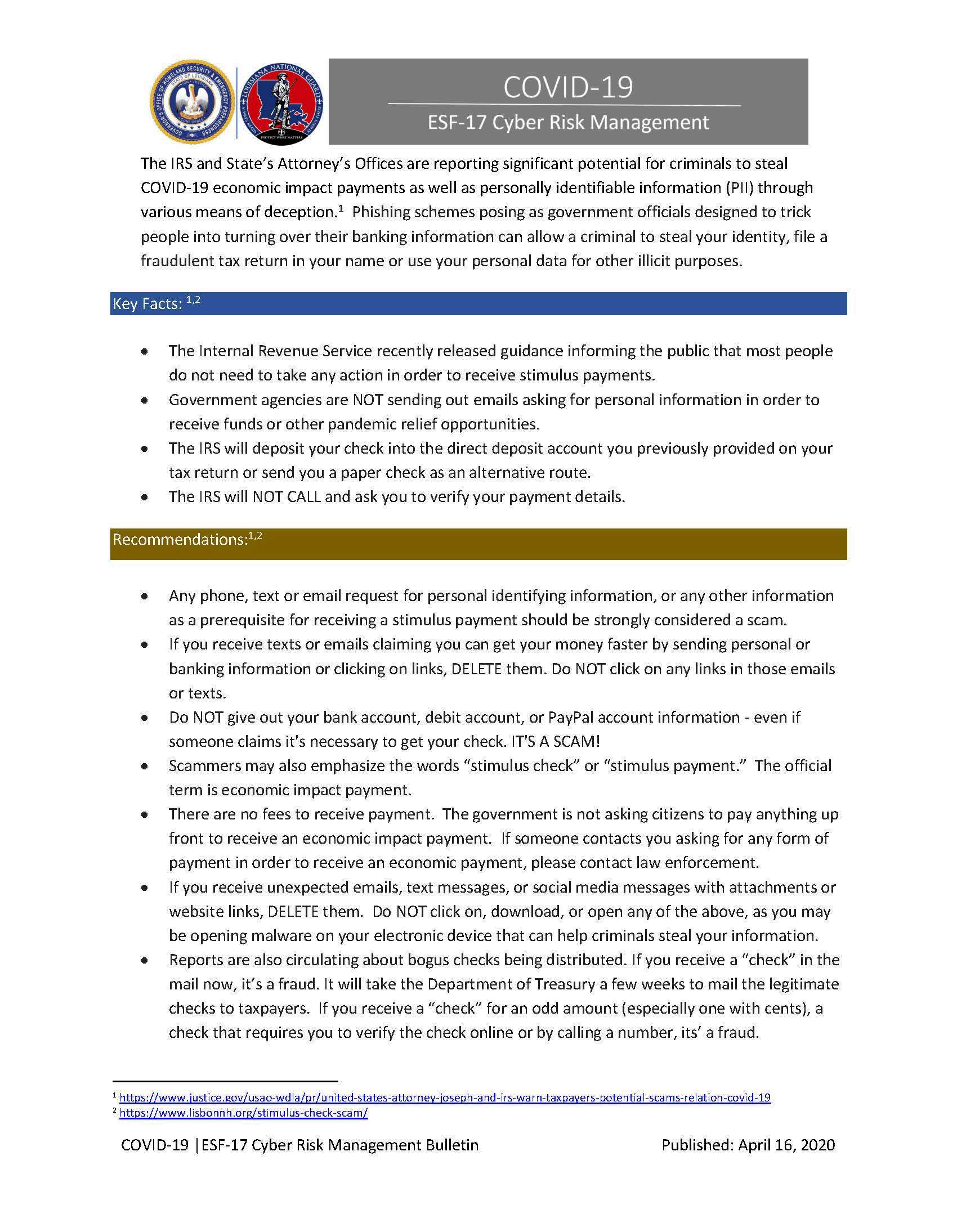
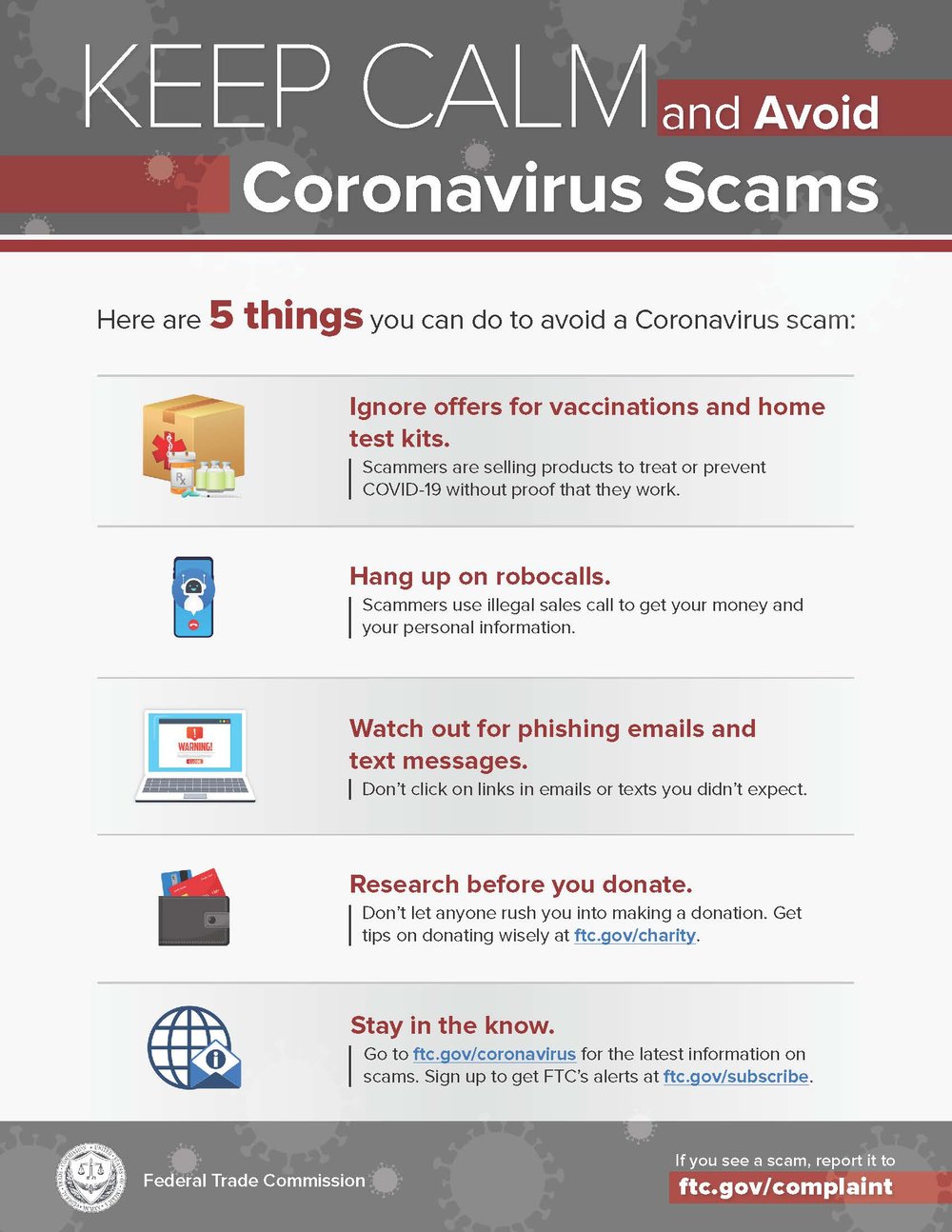
Having COVID-19 Symptoms? Here's When to Seek Medical Attention.
If you begin to develop the symptoms we are repeatedly hearing about – cough, fever and shortness of breath – it can be frightening. So how do you know which symptoms warrant medical attention?
If you wake up with a fever or a tickle in your throat, stay calm. There are many illnesses that could result in same symptoms.
It may be tempting to rush to your nearest hospital emergency room, but no matter what illness it is, you should always monitor your symptoms and seek the advice of your primary care provider FIRST. This is even more important now when hospital resources are needed for those who are truly in need of care.
Lane Family Practice: 654-3607
Lane Pediatrics: 658-4070
Lane OB/GYN: 658-1303
FASTLane Urgent Care: 570-2618
If your symptoms become more critical, then seek emergency care. The CDC currently recommends that you should seek medical attention immediately if you develop these emergency warning signs* for COVID-19:
- Trouble breathing
- Persistent pain or pressure in the chest
- New confusion or inability to arouse
- Bluish lips or face
*This list is not all inclusive. Please consult your medical provider for any other symptoms that are severe or concerning.
------------------------------------------------------------------------------------------------------------------------------------------------------
Safety Precautions

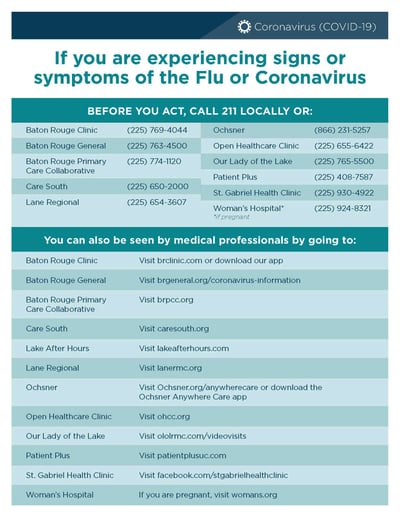
FAQs - COVID-19 (Coronavirus)
What is Coronavirus Disease 2019 (COVID-19)?
- Human coronaviruses existed before this including some that commonly cause mild upper-respiratory tract illnesses like the common cold.
- COVID-19 is a new disease, caused by a new coronavirus that has not previously been seen in humans.
- The coronavirus that causes COVID-19 likely originated in bats.
- This new coronavirus strain has the potential to cause more severe respiratory disease than previously circulating coronaviruses.
How is COVID-19 spread?
- Person-to-person spread - The virus is thought to spread mainly from person-to-person.
- Between people who are in close contact with one another (within about 6 feet).
- Through respiratory droplets produced when an infected person coughs or sneezes. These droplets can land in the mouths or noses of people who are nearby or possibly be inhaled into the lungs.
- Spread from contact with infected surfaces or objects.
- It may be possible that a person can get COVID-19 by touching a surface or object that has the virus on it and then touching their own mouth, nose, or possibly their eyes, but this is not thought to be the main way the virus spreads.
Can someone spread the virus without being sick?
- People are thought to be most contagious when they are most symptomatic (the sickest).
- Some spread might be possible before people show symptoms; there have been reports of this occurring with this new coronavirus, but this is not thought to be the main way the virus spreads.
How easily does the virus spread?
What are the Symptoms of COVID-19?
- Reported illnesses have ranged from mild symptoms to severe illnes
- The following symptoms may appear 2-14 days after exposure
- Fever
- Cough
- Shortness of breath
Who Gets Tested for the Novel Coronavirus?
- Have a fever of 100.0F or greater
- Test negative for influenza
- Be diagnosed with a lower respiratory infection
What to do if you think you are sick with COVID-19?
What About Wearing a Mask?
- Wearing a surgical mask will not keep you from getting COVID-19
- Masks are in high demand throughout the country
- Healthcare facilities are being given an allotted amount of masks
- Everyone needs to do their part to conserve masks that are not needed
What are the Best Prevention Practices?
It is important for everyone to practice these everyday precautions to help prevent the spread of germs:
- Wash your hands often - for 20 seconds with soap and water, or use alcohol-based hand sanitizer
- Cover your cough or sneeze with your elbow or a tissue
- Do not touch your face
- Clean and disinfect commonly touched objects and surfaces
- Avoid people who are sick
- Stay home if you are sick, except to get medical care
To help you determine when to seek medical care, here is a list of the most common signs and symptoms to look for:
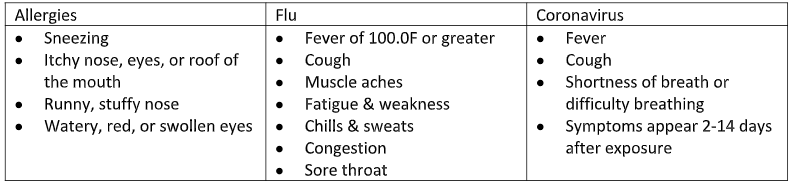



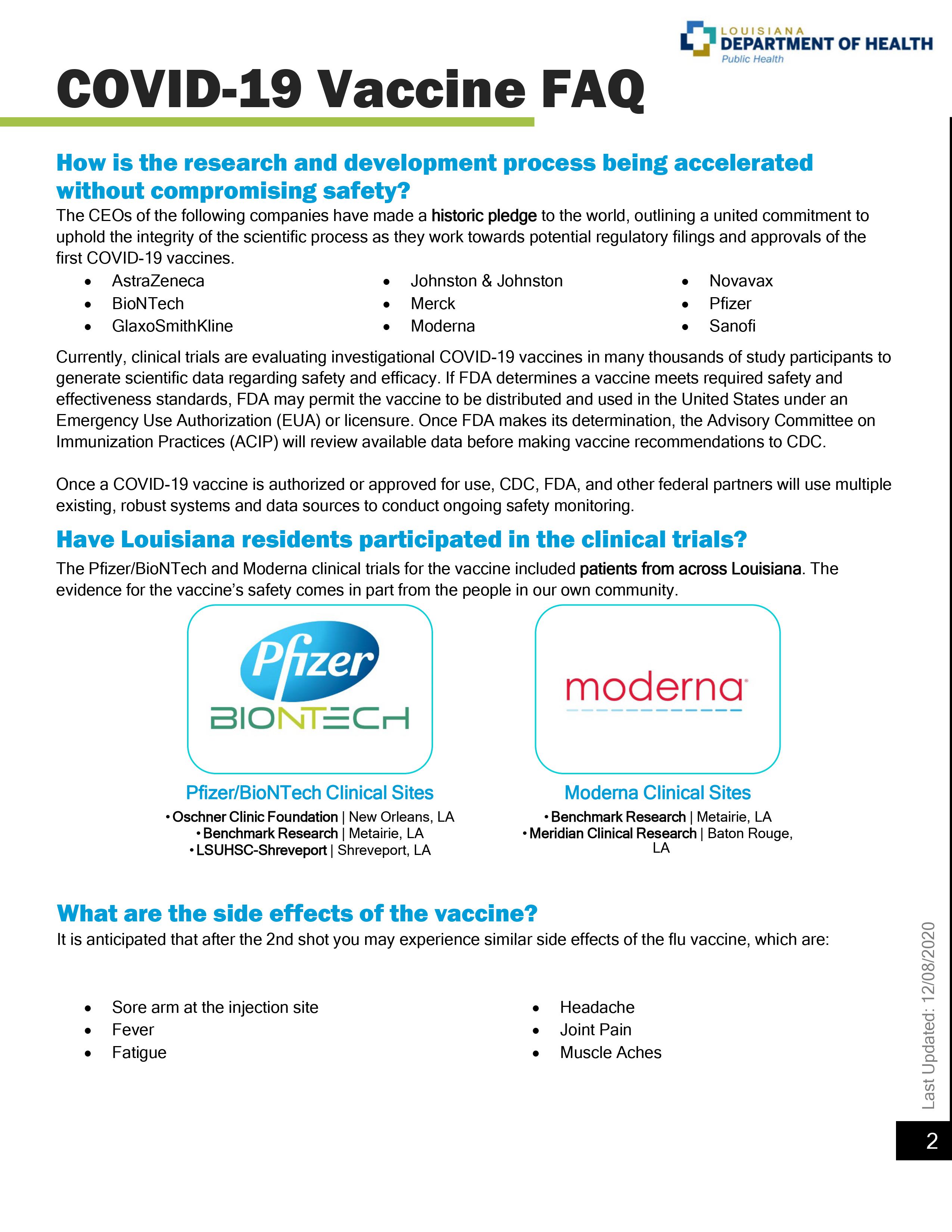
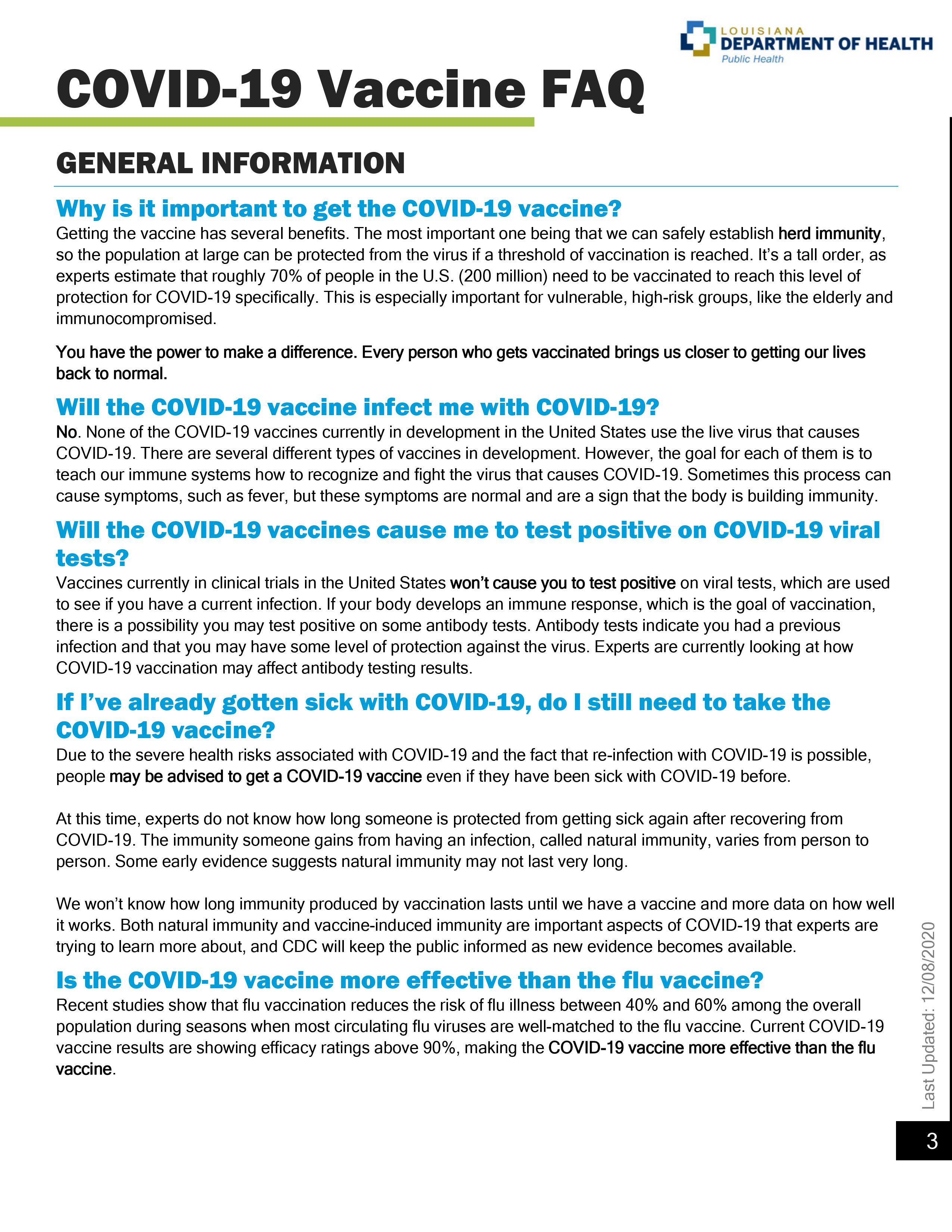
.png?width=850&height=850&name=lane%20badge%20(1).png)


-1.png?width=711&height=711&name=healthy%20br%20(4)-1.png)

